Isolated bicuspid aortic valve occurs in 0.5%–2% of the population. Reference Basso, Boschello and Perrone1-Reference Steinberger, Moller, Berry and Sinaiko3 The risk for progressive aortic stenosis, aortic regurgitation, aortic dilation, and aortic dissection underpins guidelines recommending close follow-up and imaging, medical management strategies, and activity restriction in adults. Reference Nishimura, Otto and Bonow4-Reference Doherty, Kort, Mehran, Schoenhagen and Soman6 Recent studies have shown a lower risk and slower rate of progression of aortic disease associated with bicuspid aortic valve in children as compared to adults. Reference Spaziani, Ballo and Favilli7-Reference Yamauchi, Puchalski and Weng9 Despite this research, new appropriate use criteria for imaging in children with bicuspid aortic valve recommend shorter intervals of follow-up than those recommended in earlier guidelines for adults. Reference Nishimura, Otto and Bonow5,Reference Doherty, Kort, Mehran, Schoenhagen and Soman6,Reference Sachdeva, Valente and Armstrong10
There are limited data describing management strategies in children up to age 18 years, and until this year, there were no formal guidelines for management of isolated bicuspid aortic valve in children. To correspond with the release of the first appropriate use criteria for imaging of this valvular heart disease, Reference Sachdeva, Valente and Armstrong10 this study describes current follow-up intervals and management strategies for isolated bicuspid aortic valve. Children up to and including 18 years of age were included, despite the presence of adult guidelines that would apply to the 18-year-old patients, as paediatric cardiologists often follow patients up to their mid-20s and recent appropriate use criteria were written to include 18-year-old patients. A better understanding of current clinical practice will allow for identification of areas of discordance between what is known about the course of this disease in children, follow-up recommendations, and how clinicians currently manage patients. Further exploration of these areas of discordance may guide future revisions to the current guidelines or interventions to encourage standardisation of practice.
Methods
Study design
This cross-sectional, online survey study of paediatric cardiac providers received an exemption from the University of Wisconsin Health Sciences Institutional Review Board and was administered in March and April of 2020. An initial invitation was sent on 3/11/2020, and two reminder emails were sent two and five weeks later.
Study population
Eligible participants were members of either the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery or the PediHeartNet online community with active email addresses on file. Members of these organisations include a spectrum of professionals involved in the care of children with heart disease.
Survey development
The survey contained 17 questions. Responses included numeric input as well as binary, multiple choice, and five-point Likert scale selections. Survey domains included demographic data as well as interval of follow-up; indications for intervention or exercise restriction; use of medication to manage aortic dilation and aortic regurgitation; and echocardiographic screening of relatives of children of various ages with isolated bicuspid aortic valve and various degrees of aortic stenosis, aortic regurgitation, and aortic dilation (Table 1). In all clinical scenarios, the children in question were stated to be asymptomatic. We included patient scenarios in the age groups typically cared for by paediatric cardiologists (newborns and patients at ages 1, 6, 12, and 18 years). Following initial development, the survey was reviewed for content, design, and readability and was beta-tested to establish completion time.
Table 1. Definitions of severity of aortic disease

Data management and statistical analysis
This survey was generated on the Qualtrics web-based survey platform (Qualtrics, Provo, UT). Eligible participants were emailed a secure, anonymous link to the study. Anonymised data extracted from Qualtrics was batch processed and analysed using descriptive statistical tools in Excel (Microsoft, Redmond, WA) for both continuous (mean, median, mode, range, and standard deviation) and categorical variables (percents and total counts). The significance of age-related differences in recommendations was evaluated using repeated measures ANOVA in Stata (StataCorp, College Station, TX). A p-vale of 0.05 was a priori defined as significant.
Results
Participants
The survey was sent to a total of 1777 paediatric providers through PediHeartNet and 865 through the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery. Of 239 providers who started the survey, 106 responded to at least some of the study questions. All responses to each individual question were utilised. As there is considerable overlap between membership in the two organisations, and we could not assure that all e-mail addresses were active, we could not calculate a response rate.
Demographic characteristics are shown (Table 2). Respondents were primarily from the United States (97%) with most respondents from the Midwest (30%), South (27%), and Northeast (26%). Most respondents were physicians (92%) practicing in paediatric cardiology (97%) and, excluding trainees (5% of the sample), had been in practice for an average of 17.7 +/− 11.7 years. They hailed from programmes with surgical volumes ranging from zero cases per year (22%) to more than 300 per year (43%).
Table 2. Participant characteristics

Interval for follow up
Interval for follow-up of asymptomatic children at five set ages with isolated bicuspid aortic valve and varying degrees of aortic stenosis, aortic regurgitation, and aortic dilation is shown (Fig 1). In general, closer follow-up was recommended for younger children and those with more severe disease.
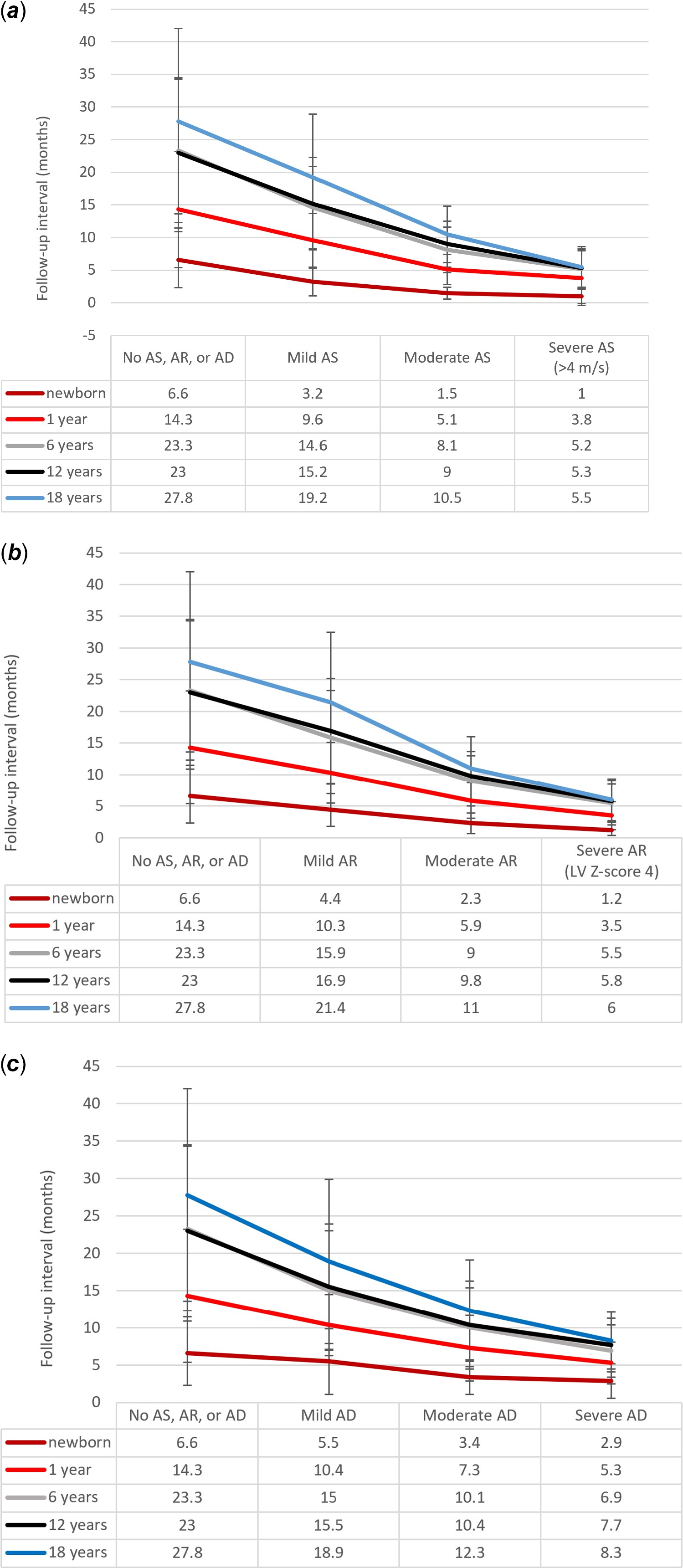
Figure 1. Follow-up intervals. Recommended interval of follow-up in months for patients with isolated BAV and varying degrees of AS (panel A), AR (panel B) and AD (panel C). AD = aortic dilation, AR = aortic regurgitation, AS = aortic stenosis.
For asymptomatic younger children (newborn or 1 year) with absent or mild aortic stenosis, aortic regurgitation, or aortic dilation, follow-up was recommended between 3 and 14 months on average, while for those patients with moderate valvular disease, follow-up was recommended between 1 and 7 months.
For asymptomatic older children (ages 6, 12, or 18 years) with absent or mild aortic stenosis, aortic regurgitation, or aortic dilation, follow up was recommended every 1–3 years on average. For asymptomatic older children with moderate aortic stenosis, aortic regurgitation, or aortic dilation, follow up was recommended every 8–10 months.
While the majority (50%–75%) of providers indicated they would recommend intervention for asymptomatic patients with severe aortic stenosis or aortic regurgitation regardless of their age (Fig 2), those providers who chose not to intervene chose an average follow-up interval of 5–6 months for patients ages 6 years and up (Fig 1). A smaller percentage of providers recommended intervention for asymptomatic patients with severe aortic dilation (25%–55% depending on the age of the patient, Fig 2). Instead, providers opted for close follow-up, ranging from 3 months for newborns to 8 months for an 18-year-old patient (Fig 1).
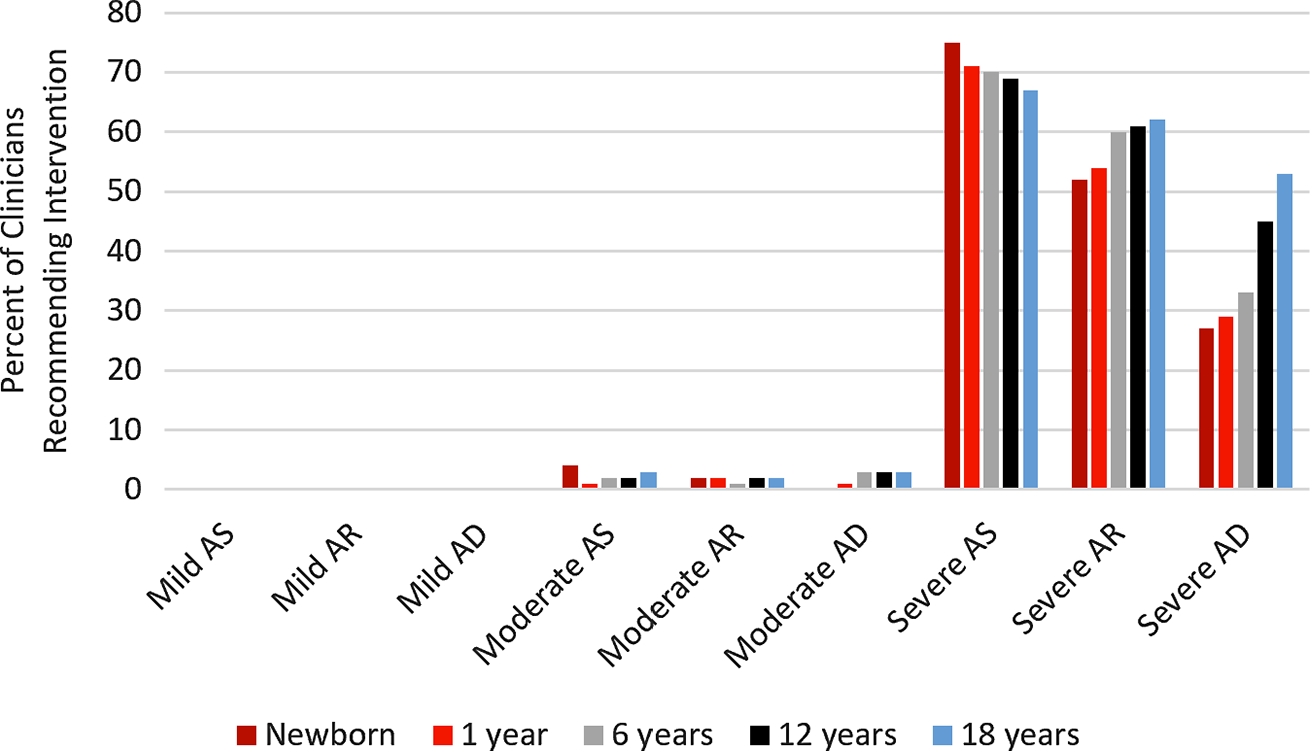
Figure 2. Indications for Intervention. Percent of clinicians recommending surgical or catheter-based intervention at different ages in patients with isolated BAV and varying degrees of AS, AR, and AD. AD = aortic dilation, AR = aortic regurgitation, AS = aortic stenosis.
Indications for intervention
Many providers do not recommend intervention for aortic stenosis or aortic regurgitation based on qualitative descriptions of valvular dysfunction in the absence of symptoms (Fig 2). No clinicians recommended intervention for asymptomatic patients with no or mild aortic stenosis, aortic regurgitation, or aortic dilation. Very few (<10%) recommended intervention for moderate aortic stenosis, aortic regurgitation, or aortic dilation. Many recommended intervention for severe aortic regurgitation (50%–60%) or aortic stenosis (65%–75%), with a greater percentage of providers recommending intervention at younger ages in aortic stenosis and a greater percentage recommending intervention at older ages in aortic regurgitation. While a slight majority of providers recommended intervention for 18-year-old patients with severe aortic dilation (55%), only a minority of providers (25%-45% depending on age) recommended intervention for younger patients with severe aortic dilation in the absence of symptoms.
The vast majority of providers recommended intervention for patients with aortic stenosis at set pressure gradients regardless of age or symptomatology (Table 3). Providers recommended intervention for any age patient at an average pressure gradient of 48+/−8 mmHg. Repeated measures ANOVA was used to explore the relationship between patient age and clinician recommendations. The same percentage of clinicians recommended intervention at some threshold even in asymptomatic patients regardless of the patient’s age (p = 0.810); however, the threshold chosen for intervention was lower in younger patients (p < 0.001).
Table 3. Intervention or exercise restrictions in asymptomatic patients with aortic stenosis

Indications for activity restriction
Providers recommended exercise/activity restrictions for asymptomatic 6-, 12- and 18-year-old patients at an average pressure gradient of 38+/−11 mmHg. Repeated measures ANOVA was used to explore the relationship between patient age and clinician recommendations. Both the recommendation for activity restriction in an asymptomatic patient (p < 0.001) and the threshold at which that recommendation would be made to restrict activity (p = 0.004) varied by age, with more clinicians recommending restriction at a lower threshold in older patients.
Use of medication
In total, 87% of providers report having used medications to manage aortic regurgitation or dilation (Table 4). Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers were the preferred medications for management of aortic regurgitation, while angiotensin receptor blockers and beta blockers were the preferred medications for management of aortic dilation (Fig 3).
Table 4. Medication recommended for management of aortic regurgitation and aortic dilation


Figure 3. Medications used in BAV. Percent of those clinicians who ever use medications for the treatment of AR and AD who recommend each of four common antihypertensives: ACEi, ARB, beta blockers, CCB. ACEi = angiotensin converting enzyme inhibitor, AD = aortic dilation, AR = aortic regurgitation, ARB = angiotensin receptor blocker, AS = aortic stenosis, CCB = calcium channel blocker.
Echocardiographic screening of relatives
In total, 82% of providers recommended echocardiographic screening of an affected patient’s first-degree relatives.
Discussion
While previous guidelines for follow-up, imaging, and intervention of isolated bicuspid aortic valve targeted adult patients, this year, appropriate use criteria for imaging follow-up of children were released (Table 5). Reference Nishimura, Otto and Bonow4-Reference Doherty, Kort, Mehran, Schoenhagen and Soman6,Reference Sachdeva, Valente and Armstrong10,Reference Bonow, Carabello and Chatterjee11 Prior to the release of these guidelines, clinicians relied on individual clinical expertise and extrapolation of recommendations from adult guidelines to guide their care of patients with this lesion. While we now have a consensus statement on the use of imaging for follow-up of this lesion; paediatric-specific exercise, Reference Boyett Anderson, Moreno and Hokanson12,Reference Baleilevuka-Hart, Teng, Carson, Ravekes and Holmes13 medical management, and interventional recommendations are still lacking.
Table 5. Timeline of recommended* frequency of imaging for management of aortic lesions

* Clinical practice guidelines (CPG) and appropriate use criteria (AUC); m = months; y = years
† If dilation <4.5 cm, stable dilation, no family history of aortic dissection
‡ i.b.i.d
§ If dilation >4 cm
** If >4.5 cm, rapid rate of change in diameter, or family history of aortic dissection
†† If >4 cm and one or more of the following: >4.5 cm, rapid rate of change in diameter, first-degree relative with aortic dissection
Follow-up intervals
In general, clinicians recommended a shorter interval of follow-up for the oldest children (age 18) with isolated bicuspid aortic valve than recommended by current clinical practice guidelines for adults regardless of the degree of valvulopathy (Figs 1 and 4, Table 5). Reference Nishimura, Otto and Bonow4

Figure 4. Clinician follow-up vs. AUC. Comparison of clinician recommendations with AUC recommendations for follow-up interval of patients with isolated BAV with AS (panel A) and AR (panel B). Survey data shown as a means for each age and degree of valvular dysfunction. AUC guidelines shown as shaded areas representing the range of intervals over which follow-up is recommended at each age for patients with mild (red) and moderate (blue) valvular dysfunction. AR = aortic regurgitation, AS = aortic stenosis, AUC = appropriate use criteria.
Follow-up intervals recommended for asymptomatic children ages 6–12 years with isolated bicuspid aortic valve and mild or moderate aortic stenosis or aortic regurgitation were comparable to those recommended in the newest appropriate use criteria for children. Despite research showing a low risk and slow rate of progression aortic valve dysfunction in children compared to adults, Reference Spaziani, Ballo and Favilli7,Reference Yamauchi, Puchalski and Weng9 the intervals recommended in the newest appropriate use criteria and those reported by clinicians were shorter than those recommended for adults (Fig 4). Reference Doherty, Kort, Mehran, Schoenhagen and Soman6,Reference Sachdeva, Valente and Armstrong10
By contrast, clinicians followed up newborns and infants with isolated bicuspid aortic valve and mild or moderate aortic stenosis or aortic regurgitation at intervals that were longer than those recommended in the new paediatric appropriate use criteria (Fig 4). Reference Sachdeva, Valente and Armstrong10 For newborns with mild valvulopathy, follow-up was reported at 3–4 months (compared to the recommended 1–4 weeks), while infants with the same severity of disease were followed up at 10 months (compared to the recommended 3–6 months). For newborns with moderate valvulopathy, follow-up was reported at 6–8 weeks (compared to the recommended 1–4 weeks), while infants with the same severity of disease were followed up at 5–6 months (compared to the recommended 1–3 months). Formulating recommendations for follow-up of these young children can be challenging as there are few patients and a paucity of data at this age range; however, the longer-than-recommended follow-up intervals reported by clinicians suggest that clinical experience has shown that the overall progression of disease in infants is not as rapid as implied by the new appropriate use criteria.
For patients with isolated bicuspid aortic valve without aortic stenosis, aortic regurgitation, or aortic dilation, surveillance imaging was recommended at significantly shorter intervals (6 months for newborns, 14 months for infants, 2 years for children) than recommended by current paediatric or adult appropriate use criterion (3–5 years, Table 5). Reference Doherty, Kort, Mehran, Schoenhagen and Soman6,Reference Sachdeva, Valente and Armstrong10
Comparison of survey data regarding aortic dilation to the new paediatric appropriate use criteria is challenging as the appropriate use criteria used different classifications than were used in this study. As with aortic stenosis and aortic regurgitation, paediatric providers followed up 18-year-olds with varying degrees of aortic dilation at approximately the same intervals as those recommended for adults, with shorter intervals recommended for younger children and those with more severe disease (Fig 1, Table 5).
Indications for intervention
Current appropriate use criteria do not offer recommendations for imaging follow-up of patients with isolated bicuspid aortic valve and severe aortic stenosis, aortic regurgitation, or aortic dilation as “it was assumed that these patients will undergo surgical or catheter-based interventions”. Reference Sachdeva, Valente and Armstrong10 This aggressive approach toward intervention does not appear to correlate with contemporary practice as our data show that between 25% (newborn with severe aortic stenosis) and 70% (newborn with severe aortic dilation) of providers would not recommend intervention in an asymptomatic child with severe aortic stenosis, aortic regurgitation, or aortic dilation.
Indications for activity restriction
While guidelines for the participation of individuals with structural heart disease in competitive athletics exist for children ages 12 years and older, there are no guidelines addressing recreational activities or athletic participation for younger patients. Reference Braverman, Harris, Kovacs and Maron14 Clinicians in this study made recommendations for younger patients with isolated bicuspid aortic valve based on pressure gradients across the valve.
Use of medication
Clinicians were split on whether or not to medically manage aortic regurgitation and aortic dilation (Table 4). While there may be a theoretical benefit to medical therapy in aortic regurgitation and aortic dilation, there are no formal recommendations regarding medical management of either of these entities for adults or children in the absence of hypertension. The most recent clinical practice guidelines for adults suggest that calcium channel blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers may have an advantage over beta blockers in the treatment of hypertension in the setting of aortic regurgitaiton; however, the theoretical advantage of beta blockers and angiotensin receptor blockers in the setting of aortic dilation has not been demonstrated clinical studies. Reference Nishimura, Otto and Bonow4 Medications preferred by clinicians in this study corresponded to these theoretical advantages (Fig 3).
Echocardiographic screening of relatives
In total, 82% of respondents recommended echocardiographic screening of first-degree relatives of patients with isolated bicuspid aortic valve. Despite the fact that 20%–30% of affected patients will have at least one family member with bicuspid aortic valve, there is not yet data on the cost-effectiveness of such screening or its impact on patient outcomes. Reference Nishimura, Otto and Bonow4
Study limitations
Given likely crossover of membership in the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery and PediHeartNet, it is impossible to calculate a response rate. While the survey was sent to a minimum of 1777 individuals through the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery, not all individuals would have been eligible to complete the study as this organisation accepts medical students and residents as members. In addition, this survey was sent out during March and April of 2020, as communities and organisations around the United States were beginning to mount dramatic COVID-19 pandemic responses and email inboxes were being flooded with daily missives about new developments. While the 106 usable responses were representative of providers from a wide swath of the country practicing at a wide range of practices, it is impossible to determine if there are any characteristics that differentiate those providers who responded to this survey from those who did not. Although unlikely, as the survey was conducted using an anonymous link to the survey, we cannot exclude the possibility that the survey was completed by individuals outside the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery and PediHeartNet or that respondents could have accessed the survey multiple times. Finally, our study was limited to isolated aortic valve disease and aortopathy and did not address mixed disease.
Conclusions
While children have been shown to have generally slower progression of aortic valve dysfunction than do adults in the setting of isolated bicuspid aortic valve, most respondents evaluate children at shorter intervals than those recommended for adults. New appropriate use criteria for children recommend follow-up of the youngest patients (newborns and infants) at shorter intervals than those reported by the clinicians in our study, suggesting that disease progression in these young patients may be slower than implied by the appropriate use criteria. Additionally, current appropriate use criteria for imaging do not provide guidance on follow-up of patients with severe valve dysfunction, despite the reality that many providers report continued observation in the absence of symptoms. Further exploration of these areas of discordance may guide future revisions to the current guidelines or interventions to encourage standardisation of practice. Other areas of exploration include the relative efficacy of various medications in the treatment of aortic regurgitation and dilation in the setting of this disease, the risks and benefits of current patterns of activity restriction, and the cost-effectiveness and clinical utility of echocardiographic screening of relatives. As we learn more, we can adjust our practice and recommendations to better align with our ever-evolving knowledge of this clinical entity.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1047951121001499
Acknowledgements
Members of the PediHeartNet online community and the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery for survey completion. Members of the University of Wisconsin Department of Pediatrics, Division of Cardiology for survey review. Ben Plunkett for survey design and administration. Xiao Zhang for statistical analysis and manuscript review.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None.














