A 3-year-old girl presented at 20 months-of-age with respiratory distress and low cardiac output. Her cardiac examination and echocardiogram confirmed severe dilated cardiomyopathy and decompensated congestive cardiac failure. She was intubated ventilated and started on intravenous inotropes. After transfer to the national paediatric cardiology unit, her echocardiogram confirmed severe dilated cardiomyopathy/myocarditis with severe LV dilatation and reduced LV systolic function (LV fractional shortening 10–15%). Initial nasopharyngeal aspirate was positive for adenovirus and rhinovirus.
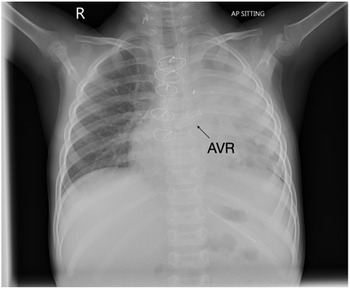
Despite escalating inotropic and mechanical ventilation support, she required placement on extracorporeal membrane oxygenation due to persistent decompensated cardiac failure despite maximal ventilatory and inotropic support. Cardiomyopathy and myocarditis work-up failed to identify an underlying aetiology. Given her need for ventricular assist device support and listing for orthotopic heart transplant, she was transferred by air ambulance to the transplant centre in Newcastle, England. Two days after arrival in the transplant centre she was placed on biventricular assist device but failed to show any recovery of ventricular function. She had a Berlin heart inserted 2 days after she was placed on biventricular assist device. She underwent orthotopic heart transplantation 3 months after transfer to transplant centre. She was initially treated with intravenous cyclosporin before transitioning to tacrolimus. Subsequently, she developed Enterococcus faecalis bacterial endocarditis resulting in severe aortic regurgitation. This was not amenable to valve repair and required aortic valve replacement (AVR) with a 19 mm On-X valve 11 days after her transplant.
She had a difficult post-transplant course and suffered several complications including malabsorption requiring nasogastric and then nasojejunal feeding, liver dysfunction, thoracolumbar osteoporotic wedging and compression fractures (treated with vitamin D), renal impairment with echogenic kidneys and adrenocortical insufficiency. She also developed several episodes of sepsis including Epstein–Barr viraemia, Burkholderia cepacia, Stenotrophomonas maltroplilia, Klebsiella oxytoca and Pseudomona aureginosa sepsis requiring several antibiotics including ceftolazone-tazobactem, micafungin and aztreonam with taurolidine nebulizers. She developed a pulmonary haemorrhage soon after her transplant and needed tracheostomy for left main stem bronchomalacia. Although she was decannulated she developed respiratory distress with repeated respiratory infections and subsequently needed her tracheostomy site reopened. Her most recent echocardiogram demonstrated good aortic valve function. She was anticoagulated with warfarin (On-X valve INR 2-3 for first 3 months; INR 1.5-2.0 thereafter).
This is the first reported aortic valve replacement in a child after cardiac transplantation using an On-X valve. Although attempted repair was contemplated, the valve destruction was too severe warranting replacement. Given the size of the donor heart, it was possible to implant 19 mm valve in this 12 kg child with minimal risk of patient prosthesis mismatch. Her most recent echocardiogram demonstrated excellent prosthetic valve function with mild para-valve regurgitation, mild LV dilatation, global longitudinal strain -19% and left ventricular ejection fraction 60% (Simpson’s biplane). Benefits of the On-X valve include its unique material and design characteristics compared with earlier generations of mechanical valve. The valve also can be used safely with less anticoagulation (INR 2-3 for first 3 months; INR 1.5–2 thereafter). (1). In a prospective randomized trial, patients using lower dose anticoagulation had at least 60% fewer bleeding events without any increase in their stroke risk (2). Furthermore, the valve has a much lower reoperation risk compared to bioprosthetic tissue valves. This report highlights the potential for successful outcome of AVR using the On-X valve post orthotopic heart transplant despite significant co-morbidities in this patient.
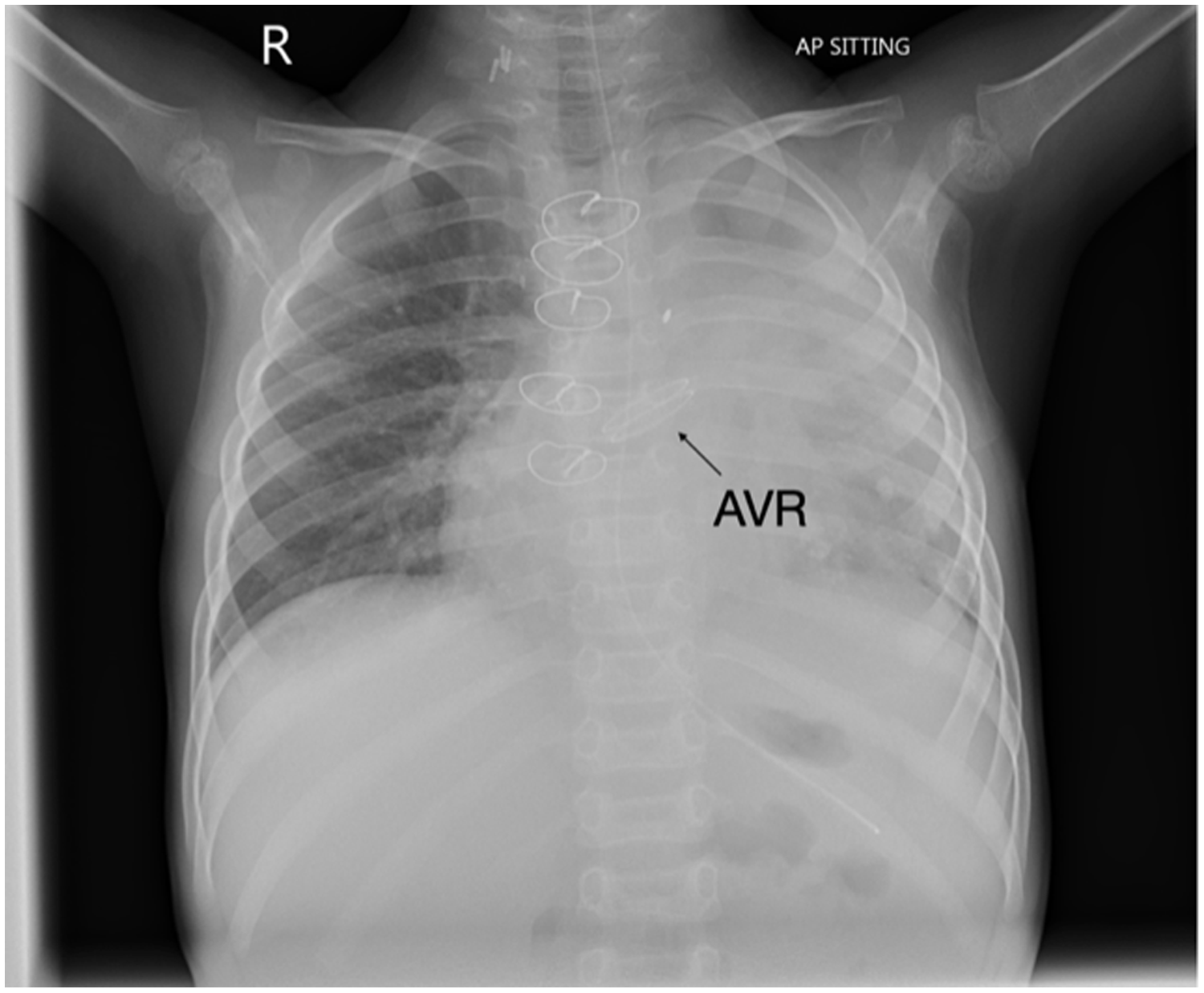
Figure 1. Chest radiograph demonstrating bileafelt On-X aortic valve.

Figure 2. Transthoracic echocardiogram four chamber view demonstrating On-X valve in situ.
Acknowledgements
We would like to express our gratitude to Mr. John Russell, ENT surgeon and Ms. Marie Lavelle, Department of Paediatric Cardiology and Cardiac Transplantation, Children’s Health Ireland. Mr Andrew Pendred kindly generated the images.
Financial support
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflicts of interest
None