Introduction
Approximately 30% of patients with major depressive disorder (MDD) are nonresponders to multiple consecutive trials of antidepressants,Reference Rush, Trivedi and Wisniewski1 and more than half of these patients are nonresponders to electroconvulsive therapy (ECT).Reference Heijnen, Birkenhäger and Wierdsma2 Fifteen percent of patients seeking help for obsessive–compulsive disorder (OCD) consider themselves disabled, and approximately 40–60% fail to respond to selective serotonin reuptake inhibitors and to clomipramine.Reference Drubach3 Treatment resistance leads to reduced quality of life,Reference Bouwmans, Vemer and van Straten4–Reference Ishak, Balayan and Bresee6 increased risk of suicide,Reference Borges, Angst and Nock7, Reference De La Vega, Giner and Courtet8 and decreased work productivity.Reference Alonso, Petukhova and Vilagut9
Recent studies have shown that up to 60% of patients suffering from treatment-resistant OCD (TR-OCD) respond to deep brain stimulation (DBS),Reference Alonso, Cuadras and Gabriels10, Reference Graat, Figee and Denys11 up to 41% respond to anterior cingulotomy, and up to 54% respond to anterior capsulotomy.Reference Brown, Mikell and Youngerman12 Open-label trials have resulted in 30–50% remission rates for DBS in treatment-resistant MDD (TR-MDD)Reference Lozano, Mayberg and Giacobbe13–Reference Schlaepfer, Bewernick and Kayser18 although two randomized controlled trials (RCTs) have had conflicting resultsReference Bergfeld, Mantione and Hoogendoorn19, Reference Dougherty, Rezai and Carpenter20 and a recent multisite randomized sham-controlled trial has failed to demonstrate statistically significant benefits.Reference Holtzheimer, Husain and Lisanby21
Anterior cingulotomy and capsulotomy consist of making small lesions in the anterior cingulate gyrus and the anterior limb of the internal capsule, respectively. Symptom reduction is believed to result from disruption of signaling in the excitatory orbito-fronto-thalamic and inhibitory cortico-striato-thalamo-cortical circuits.Reference Shah, Pesiridou and Baltuch22 The procedure is most often accomplished by burr-hole introduction of electrodes at the target site to produce a thermal lesion, a technique termed thermocoagulation. More recently, anterior capsulotomy has been performed using gamma knife-focused ionized radiationReference Meng, Suppiah and Mithani23, Reference Rasmussen, Noren and Greenberg28 and MR-guided focused ultrasoundReference Jung, Kim and Roh24 to produce very precise stereotactic lesions. These techniques are considered less invasive as they do not require open surgery.
DBS is a neurosurgical intervention that was first employed in the 1970s and has been most widely used in the treatment of movement disorders such as Parkinson’s disease and essential tremor, but its positive effects on mood and anxiety symptoms has led researchers to study its efficacy for psychiatric disorders. DBS consists of implanting electrodes in target areas deep within the brain (i.e. subcallosal cingulate gyrus, thalamus, subthalamic nucleus, anterior limb of the internal capsule, globus pallidus, and nucleus accumbens). The electrodes are connected to a pulse generator that is implanted underneath the skin of the chest wall. Parameters can be adjusted to modulate brain activity, and stimulation can be interrupted at any time to reverse undesired side effects. The exact mechanisms of action are not clearly established, but DBS is thought to exert its effects at both neuronal and network levels by increasing neurotransmitter release, modulating neuronal synchronization, and promoting neuroplasticity.Reference Anderson, Frye and Abulseoud25
Adverse effects of anterior cingulotomy/capsulotomy (AC) and DBS are usually mild and/or transient,Reference Alonso, Cuadras and Gabriels10, Reference Graat, Figee and Denys11, Reference Anderson, Frye and Abulseoud25–Reference Rasmussen, Noren and Greenberg28 and unlike older neuroablative techniques such as leucotomies and lobotomies,Reference Feldman and Goodrich29, Reference Volpini, Giacobbe and Cosgrove30 major complications are rare occurrences.Reference Anderson, Frye and Abulseoud25
While symptom relief and even remission can sometimes be obtained in patients with TR-MDD and TR-OCD,Reference Anderson, Frye and Abulseoud25, Reference Pepper, Hariz and Zrinzo26 there are very few patients undergoing these neurosurgical procedures.Reference Pepper, Hariz and Zrinzo26 Many factors could explain this, including administrative barriers, limited resources, and resistance from psychiatrists and other clinicians in referring potential candidate patients.
The proportion of psychiatrists referring eligible patients for neurosurgical procedures is currently unknown. We hypothesized that most of them would not feel comfortable referring patients for DBS or AC mainly because of a lack of knowledge regarding these procedures. Researchers also question a contribution of social stigma and persistent fear attached to neurosurgical interventions, given historical transgressions and harsh complications having resulted from older ablative procedures performed in the mid-1900s.Reference Shah, Pesiridou and Baltuch22, Reference Feldman and Goodrich29, Reference Volpini, Giacobbe and Cosgrove30
A few studies have identified factors associated with a positive attitude toward ECT (i.e. being a doctor, higher perceived level of knowledge).Reference Jaffe, Shoyer and Siegel31, Reference Dauenhauer, Chauhan and Cohen32 However, this study is the first to evaluate the attitudes and perceptions of psychiatrists and psychiatry residents regarding neurosurgical interventions, specifically DBS and AC, for treating psychiatric disorders. It aims to identify potential barrier to patient referral.
Methods
Population
All residents enrolled in a psychiatry residency program in the province of Quebec (n = 276) and psychiatrists practicing at either one of the two affiliated centers, McGill University Health Center or Centre hospitalier universitaire de Sherbrooke (n = 159), received invitation emails to participate in the study. As stated in the recruitment email, completion of the survey by participants was considered as implied consent. The only exclusion criteria consisted of a survey completion of less than 25%. The opinion of all psychiatrists, including child and geriatric psychiatrists, was considered important as the survey collected data not only on the referral patterns but also on the interest of psychiatrists in attending conferences to enhance their knowledge on neurosurgical procedures.
Procedure
The study was reviewed for ethical compliance and approved by the McGill University Health Center’s Research Ethics Board. The researchers asked for help from the Departments of Psychiatry at McGill University and Université de Sherbrooke and from the Fédération des médecins résidents du Québec (FMRQ) to send invitation emails to psychiatrists and residents. Two reminder emails were sent at 3-week intervals in order to recruit as many participants as possible. The survey took place between December 2017 and February 2018. The survey was completely voluntary, and there were no financial incentives to completing it. Participants could stop answering questions at any time. No direct contact between participants and authors was initiated. The survey remained confidential with no identifying information.
Tools
A survey consisting of 25 questions was created by the researchers using SurveyMonkey and was distributed in French and English versions. The survey was developed by the first author, and then assessed for face and content validity by all other authors, after which improvements were implemented. In order to prevent duplicate responders, participants could answer only once from their computer as SurveyMonkey would block any second attempt coming from the same device. Participants could only access the survey through their university email.
Subjects were asked a set of questions relating to sociodemographic variables (i.e. age, gender, and professional status) and characteristics of their clinical practice (i.e. environment of practice, main area of interest, and number of active TR-MDD and TR-OCD patients). A 10-item list in which participants could select multiple items was displayed in order to identify potential barriers to referral.
Patterns of referral to DBS and AC were evaluated using 5-point Likert scales (1 = I would strongly discourage this type of intervention, 5 = I would strongly encourage this type of intervention). There were also 5-point Likert scale questions evaluating the level of agreement or disagreement (1 = strongly disagree, 5 = strongly agree) with certain statements thought to influence their attitudes toward referral. Scores of 1 or 2 were considered as disagreement, while scores of 4 or 5 were considered as agreement and a score of 3 was considered as neutral. The final set of Likert-type questions inquired about how participants perceive their level of knowledge and interest in acquiring more information on neurosurgical therapeutic modalities. Participants were free to add narrative comments throughout the questionnaire. French comments were translated to English by the researchers.
A copy of the survey can be found in the supplementary material section.
Statistical Analyses
Descriptive statistics are presented as the number of respondents and valid percentage (n = 99 unless otherwise specified). The impact of the psychiatric condition and neurosurgical procedure on the respondent’s tendency to refer was assessed using the Friedmann test, which is a variant of the one-way ANOVA used to compare groups with multiple measures when the dependant variable is ordinal in nature (i.e. Likert scales).33 IBM SPSS Statistics, version 25 (IBM, Armonk, New York), was used to perform all analyses.
Results
Demographics of Survey Respondents
From the 435 email recipients (159 psychiatrists and 276 residents), a total of 106 responses were collected, yielding a 24% response rate. Seven participants completed less than 25% of the survey and were excluded from data analysis as only demographic information and questions pertaining to their clinical practice had been answered. In total, 35 psychiatrists (35.35%) and 64 residents (64.64%) were included in the study (see Table 1 for sociodemographic data).
Table 1: Sociodemographic variables of the participants
Among the 35 psychiatrists, 18 (51.43%) were currently following at least 1 patient with TR-MDD (i.e. resistance to psychotherapy, multiple lines of pharmacotherapy, adjuvant pharmacotherapy, and ECT or repetitive transcranial magnetic stimulation (rTMS)) or TR-OCD (i.e. resistance to psychotherapy and multiple lines of pharmacotherapy including clomipramine and adjuvant medications). From the group of 18 psychiatrists following either TR-MDD or TR-OCD patients, 6 psychiatrists were following only TR-MDD patients, 3 were following only TR-OCD patients, and 9 psychiatrists were following both TR-MDD and TR-OCD patients. Four out of the 35 psychiatrists (11.43%) acknowledged having referred patients for AC or DBS during their professional career. These referring psychiatrists were following between 3 and more than 15 patients with TR-MDD and/or TR-OCD in their clinical practice.
Barriers to Referral
All respondents identified at least one barrier to referral. The cumulative percentage of participants with respect to the number of barriers selected is shown in Table 2. The majority (n = 57) identified ≥6 barriers to referral.
Table 2: Cumulative percentage of participants with respect to the number of selected barriers to referral
The list of barriers along with the number of participants having selected each barrier is presented in Table 3. The predominant barriers consisted of a lack of knowledge on the technical aspects of the procedures (n = 82), on the response and remission rates (n = 71), on the potential side effects (n = 71), and on the eligibility criteria (n = 69); administrative limitations on the referral process (i.e. how to refer) (n = 70) and on the performing centers (n = 51); fear of irreversible consequences (n = 59); and patient/family resistance to undergo neuromodulation/neuroablation (n = 57). Feeling ill at ease to discuss neurosurgery with patients (n = 19) and being unaware that neurosurgeries were still being performed for psychiatric disorders (n = 13) were also of concern to psychiatrists and residents. Eleven respondents added narrative comments. Additional barriers drawn from these comments included a lack of clear diagnostic criteria for TR-MDD and TR-OCD (n = 2), a lack of consensus on the eligibility criteria (n = 1), complex psychosocial and psychodynamic factors adding to treatment resistance (n = 2), having observed modest neurosurgical outcomes from previous referrals (n = 1), not having exhausted other less invasive interventions (n = 2), personal experience of refusal (n = 1), and limited modeling from supervising psychiatrists (n = 1).
Table 3: Barrier selection by participants
In total, 91 participants identified lack of knowledge as a barrier (i.e. in relation to the procedures, response/remission rates, side effects, or referral process). From the eight respondents (7 psychiatrists and 1 R6 resident) who did not identify this type of barrier, two acknowledged having referred patients for DBS or AC during their professional career. The tendency of participants to refer patients for a neurosurgical procedure depended on both the psychiatric condition and the type of procedure (Friedmann p < 0.0005) as summarized in Figure 1. For patients suffering from TR-OCD, 49/98 (50.00%) participants would discourage them from undergoing AC, while 52/98 (53.06%) would encourage them to undergo DBS. For patients suffering from TR-MDD, 70/98 (71.42%) would discourage them from undergoing AC. Most (47.47%) would neither discourage nor encourage DBS for TR-MDD patients.
Figure 1: Tendency of participants to encourage neurosurgical procedures for TR-OCD and TR-MDD.
Level of Agreement with General Statements
From a total of 98 participants having answered the following sets of questions, 34 subjects (34.69%) felt that DBS and AC were dangerous, 8 (8.16%) felt it was unethical to perform the procedures, and 11 (11.22%) feared a risk of abuse by professionals. Eighty-one respondents (82.65%) considered their level of knowledge on DBS and AC to be weak or poor (i.e. Likert scores of 1 or 2), 68 (69.39%) displayed an interest in attending conferences to learn more about these surgical interventions (i.e. Likert scores of 4 or 5), and 81 participants (82.65%) felt it would be pertinent to hold courses on neurosurgical procedures during residency training (i.e. Likert scores of 4 or 5) (see Figure 2). When subdividing participants according to their professional status (63 residents and fellows versus 35 psychiatrists), residents and fellows were slightly more interested (71.43%) in learning about DBS and AC than psychiatrists (65.71%).
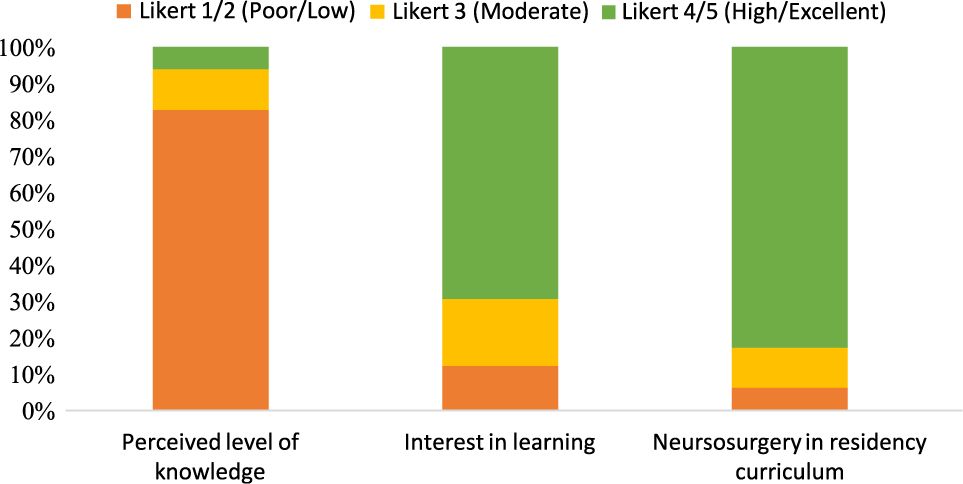
Figure 2: Participants perceived level of knowledge, interest in learning, and opinion regarding curricular inclusion of neuromodulation/neuroablation.
Qualitative Data
Eighteen participants (18.18%) added narrative comments. They expressed some similar and some differing views with respect to three main themes as described in the following:
Complexities of Psychiatric Diagnosis and Management
Participants commented on the important role of psychosocial stressors as contributors to treatment resistance in MDD and feared that neurosurgical procedures would be targeting solely biological mechanisms instead of focusing on improving patient access to health-care resources and psychosocial services.
…The clinical picture is also generally quite complicated by social stressors that would not go away with surgery and compound the clinical picture… (Participant #34E)
I can certainly see a risk of over diagnosing treatment-resistant depressive disorders when psychosocial rather than medico-surgical therapeutic frameworks should be emphasized. In a more socio-political context, I think that research funds and health care decisions are not focused enough on improving access to psychosocial services. (Participant #35F)
Participants also worried about the invasiveness of DBS and AC procedures and of referring patients too early in the process when other nonsurgical modalities might still offer benefit.
I would not feel confident that the psychopharmacological management has been optimized until I have obtained a consultation in psychopharmacology. (Participant #23E)
…It remains difficult to envision such invasive treatments when the nature of the disorder itself is not fully understood… (Participant #37F)
Gamma knife might be less frightening to patients and psychiatrists. (Participant #57F)
Continuing Education
Some felt a need for continuing education in the field of neurosurgical procedures, while others feared that too many curricular activities would focus on these treatment modalities at the expense of teaching a more holistic bio-psycho-social model of the human being.
The risk benefit ratio for these intervention is not clearly established. Surely we will need continued education before psychiatrists agree to go forward with these interventions. (Participant #21F)
Hopefully psychiatry residency training will not focus solely on neurosciences and neurosurgery when the basis of human understanding and of psychotherapeutic approaches are insufficiently covered during training. (Participant #26F)
Interdisciplinary Programs for Neurosurgical Referrals
Finally, participants perceived a need for structured interdisciplinary programs to evaluate eligible patients and support them throughout the process.
I think that a patient being considered for psychosurgery should undergo an evaluation by a multidisciplinary team that would include at the minimum an expert in psychopharmacology and an expert in psychotherapy, not an independent evaluation but a true interdisciplinary team that would agree on a treatment plan and timeframe. (Participant #23E)
We would benefit from a formal interdisciplinary provincial committee where potential cases can be referred. (Participant #33E)
Discussion
This study was the first to our knowledge to gather the opinion of psychiatrists and psychiatry residents on neurosurgical procedures for treating psychiatric disorders. We focused on DBS and AC as these procedures are currently being performed for clinical and research purposes in Quebec tertiary care centers.
Overall, psychiatrists and residents are statistically significantly more comfortable in referring patients suffering from TR-OCD than from TR-MDD. This pattern could be a reflection of the strength of evidence found in the literature currently supporting neurosurgical procedures for TR-OCD but not yet for TR-MDD. However, lack of knowledge on the response and remission rates and on the possible side effects were identified as barriers by 71.72% of participants and does not support this incline in referrals. We hypothesize that some psychiatrists might perceive a greater influence of neuronal circuitry pathology in the pathophysiology of OCD which might lead to a greater tendency to refer these patients. Future studies could try to identify the factors leading to this pattern of referral.
In addition, residents and psychiatrists preferred to refer patients for DBS rather than for AC. Although there seems to be comparable rates of side effects between these procedures, this inclination toward DBS was also outlined in another studyReference Pepper, Hariz and Zrinzo26 and might be due to the fact that DBS is a reversible procedure, albeit more invasive. One participant stated that he would feel more comfortable referring a patient for AC if the procedure was performed using gamma knife instead of thermocoagulation. Newer technology might therefore be viewed as safer and more acceptable than older ablative procedures.
In total, 18 psychiatrists (51.43%) had at least 1 patient with TR-MDD or TR-OCD in their clinical practice, but only 4 (11.43%) acknowledged having ever referred a patient for DBS or AC. This resistance to referral displayed by psychiatrists and residents might be contributing to the low number of patients undergoing these procedures worldwide. And their possible lack of knowledge on the eligibility criteria might be contributing to a high number of referred patients not meeting the requirements for the procedures.
Only seven psychiatrists had not identified lack of knowledge as a barrier to referral. Two out of the four psychiatrists having referred patients for neurosurgical evaluations during their professional career belonged to this group suggesting a positive trend toward referrals in more informed respondents, mirroring the results of the ECT literature.Reference Jaffe, Shoyer and Siegel31, Reference Dauenhauer, Chauhan and Cohen32 Also, seven out of the eight respondents who did not identify lack of knowledge as a barrier were psychiatrists, reflecting a lack of education on neurosurgical interventions during residency training.
Side effects from AC and DBS remain reasonably low and are usually transient.Reference Alonso, Cuadras and Gabriels10, Reference Graat, Figee and Denys11, Reference Pepper, Hariz and Zrinzo26–Reference Rasmussen, Noren and Greenberg28 Still, 34/98 (34.69%) participants feel that these procedures are dangerous and 8/98 (8.16%) believe that it is unethical to perform them. Research has shown that psychiatrists hold similar stigmatizing attitudes toward mentally ill individuals as the general population.Reference Schulze34 Authors thereby question a persistent social stigma attached to neurosurgical procedures, as historical disregard and complications from lobotomies and other ablative procedures have been the subject of many ethical debates over the past century with much accompanying sensationalism in movies and documentaries. The fact that 11/98 (11.22%) participants continue to fear abuse from the procedures supports this view. However, given how preliminary is our understanding of the complex neurocircuitry dynamics in MDD/OCD, there is some validity to adopting a very cautious approach in experimenting with neurosurgical procedures. Conflicting results of recent randomized controlled and randomized sham-controlled trials in demonstrating efficacy of DBS in TR-MDDReference Graat, Figee and Denys11, Reference Bergfeld, Mantione and Hoogendoorn19–Reference Holtzheimer, Husain and Lisanby21, Reference Youngerman and Sheth35 encourage clinicians to avoid falling for overhyped procedures based solely on small open label studies. In order to improve the overall knowledge and clinical acceptance of these procedures, there is a need to first improve the quality of the evidence through future modified RCTs.
One of the most striking findings in this study is that each and every participant had at least one barrier to patient referral and this attitude appears to stem predominantly from a lack of knowledge on neurosurgical procedures. Lack of adequate RCTs was not included as a separate item in the list of barriers as the authors did not want to insinuate that there was a known lack of evidence from the literature but rather to verify the participants’ current knowledge and understanding of neurosurgical interventions for treating psychiatric disorders. It is interesting to note that very few participants added this as an additional barrier. This could reflect once again a general lack of knowledge surrounding these procedures, including a lack of knowledge regarding the level of evidence supporting these interventions.
Another stated barrier was the fear of not having exhausted other less invasive treatments before resorting to neurosurgery. This mirrors the results from Garnaat et al.Reference Garnaat, Greenberg and Sibrava36 showing that from an initial group of patients with severe OCD, very few will eventually meet the inclusion criteria required to undergo DBS. Although this is a minority view, there is still a nonnegligible group of psychiatrists who view these treatments as unethical. This stance could inhibit them from referring eligible treatment-resistant patients in desperate need of last line therapeutic options.
Overall, psychiatrists and residents are interested in learning more about the procedures. Offering conferences or courses on DBS and AC during residency training might help them better inform their patients when they inquire about these treatment options and support them throughout the referral process, potentially improving overall patient care. Increasing knowledge and awareness has been shown to positively affect clinician attitudes toward mentally ill patientsReference Schulze34 and might also help lower stigmatized views of these procedures. Continuing education could be worthwhile for all residents and psychiatrists, as even senior residents studying for their Royal College examinations and psychiatrists working in child and geriatric psychiatry were interested in enhancing their knowledge on the topic.
Limitations
Some of the limitations of the study included a small number of participants, an imbalance between the number of psychiatrists and residents, and the fact that participants were only from Quebec. Having a larger number of participating psychiatrists would have permitted better comparison between residents and psychiatrists and between psychiatrists practicing in academic versus nonacademic centers, but the sample was too small to produce valuable comparisons. Because of the very low number of psychiatrists having referred patients for DBS or AC (n = 4), it was impossible to establish correlations with any of the variables. Future studies with larger sample sizes might enable profile descriptions of referring versus non-referring clinicians with regards to their area of practice, number of years of practice, perceived level of knowledge, and number of barriers to referral. It would also be interesting to evaluate differences in the attitudes of residents toward patient referral in programs where there is formal training on neurosurgical procedures.
The sample could be biased, as only 24% of the targeted population responded to the survey. These participants could be relatively more open to neurosurgical interventions than those who did not participate in the study. Also, the majority of psychiatrists who participated in the survey were younger than 50 years of age. It is possible that older psychiatrists might have a more negative view of neurosurgery for treating psychiatric disorders.
Also, this study collected data on attitudes in common to DBS and AC, but did not differentiate the two types of procedures. Given that DBS is a reversible procedure and AC an irreversible procedure, differential attitudes are expected. Future studies could analyze more precisely the differences in attitudes toward stimulation versus ablative procedures.
Finally, the Likert scales used to collect information offer a certain degree of categorization but can limit spontaneous elaboration from participants. A qualitative study asking more open-ended questions might have opened the door to other barriers.
Conclusions
In our sample, 51.43% of psychiatrists followed at least one patient with TR-MDD or TR-OCD, yet only 11.43% had ever referred a patient for neurosurgical consultation. Respondents identified lack of knowledge, administrative limitations, fear of irreversible consequences, and patient/family resistance as the main barriers to referral. Both psychiatrists and residents demonstrated a strong interest in enhancing their knowledge on these therapeutic modalities. While further research remains necessary to refine and improve the outcomes of neurosurgical interventions for treating psychiatric disorders, a significant effort on education and training will also be required for psychiatrists to consider these neurosurgical procedures in TR-MDD and TR-OCD and to view them as safe, effective, and ethically acceptable treatments.
Supplementary material
To view supplementary material for this article, please visit https://doi.org/10.1017/cjn.2019.5.
Acknowledgements
We are grateful to the Department of Psychiatry at McGill University, the Department of psychiatry at Université de Sherbrooke, and the Fédération des médecins résidents du Québec for their help in distributing our survey to psychiatrists and residents.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
conflict of interest
The authors declare that there is no conflict of interest.