A 68-year-old female presents with recent onset of bilateral sequential no-light-perception vision secondary to presumed giant cell arteritis. The patient had markedly elevated CRP/ESR (CRP 51.2 mg/L (normal <1 mg/L) and ESR > 130 mm/hr (normal <30 mm/hr)). The patient received IV methylprednisolone. Neither temporal artery could be palpated. Only the preauricular portion of the right temporal artery had a faint pulse and a biopsy in this area was deemed unsafe due to the risk of facial nerve injury. Reference Shin, Shin, Lee, Koh and Song1 On ultrasound, the arteries were nonaudible. High-resolution scalp vessel wall magnetic resonance (MR) imaging at 3T was subsequently performed and demonstrated enhancement and thickening of the wall in the proximal segment of the right superficial temporal artery which was congruent with a diagnosis of giant cell arteritis. Immediate treatment with prednisone led to improvement of her constitutional symptoms; however, she had no significant recovery of vision. High-resolution scalp vessel wall MR imaging is a recently developed technique that has been applied to the diagnosis of giant cell arteritis. Reference Rheaume, Rebello and Pagnoux2,Reference Poillon, Collin and Benhamou3 Wall thickening and enhancement of the scalp arteries are key imaging features for the diagnosis of giant cell arteritis. Reference Rheaume, Rebello and Pagnoux2 Usage of 3D techniques rather than 2D techniques has also been shown to increase sensitivity. Reference Poillon, Collin and Benhamou3 Scalp vessel wall MR imaging can be helpful in cases precluded from temporal artery biopsy for the confirmation of diagnosis (Figure 1).
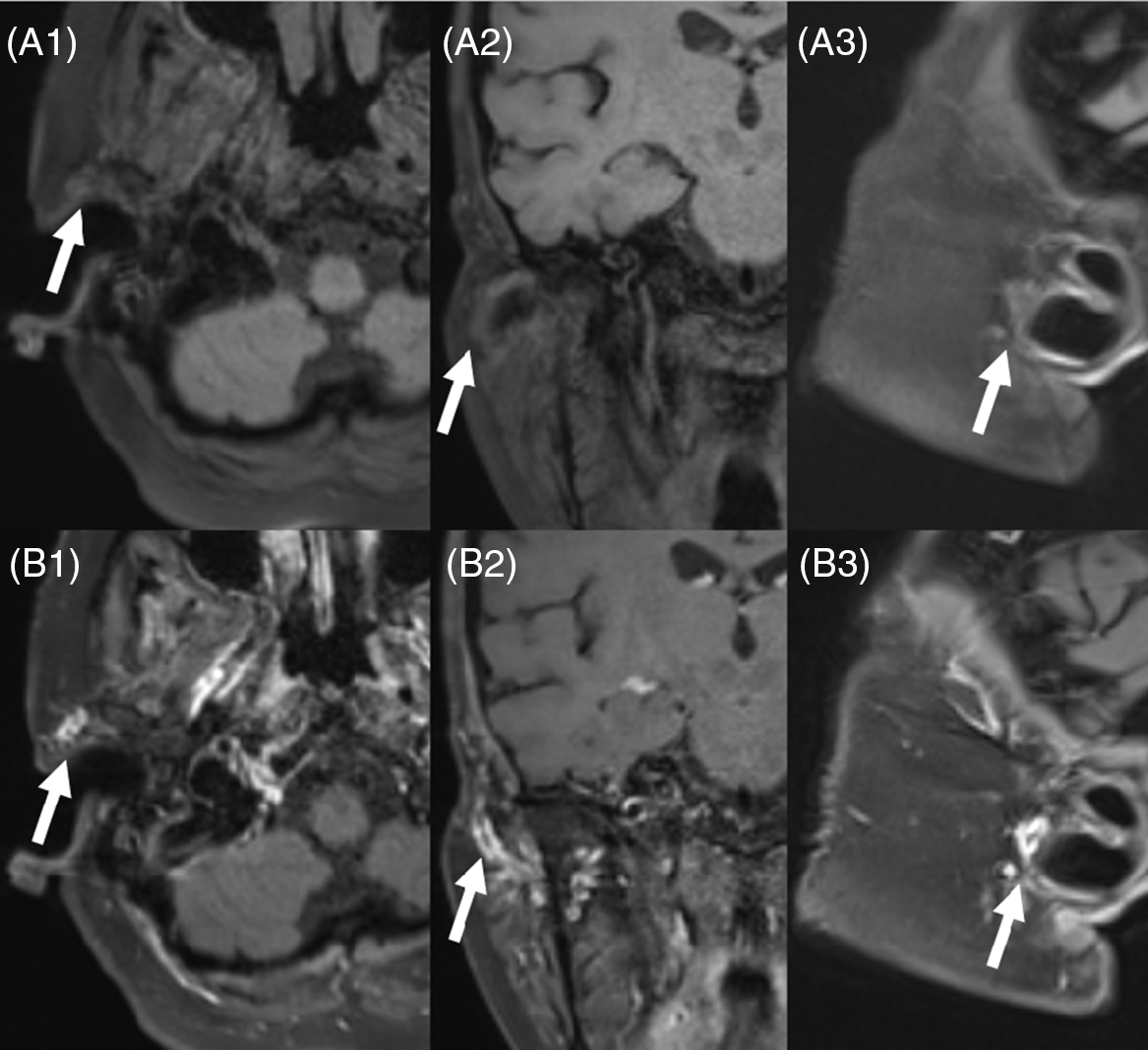
Figure 1: Pre- (A1–A3) and post- (B1–B3) contrast high-resolution MR 3D T1 FS Black Blood Images of the scalp vessels (in axial, coronal, and sagittal planes) demonstrate enhancement and thickening of the wall in the proximal segment of the right superficial temporal artery (arrow) in the region of palpable pulse.
Disclosures
The authors have no conflicts of interest to declare.
Statement of Authorship
BK, OI, DT, and MtH wrote and edited the manuscript.





