INTRODUCTION
Paul Atkinson (@eccucourse)
This series of editorials will provide CJEM readers with the opportunity to hear differing perspectives on topics pertinent to the practice of emergency medicine. The debaters have been allocated opposing arguments on topics where there is some controversy or perhaps scientific equipoise.
We continue with the topic of triage in emergency medicine. To triage or to sort is clearly a core component of any emergency assessment. Few medical systems have the resources to assess and treat each and every patient immediately on arrival at the point of care. Yet, do our current triage tools help us sort patients, or do they add unnecessary complexity and delays to the assessment process? Does formal triage help us choose who should avail of limited resources sooner, or does it drain an already overburdened system of precious resources that could be better used to support definitive care? Is a longer triage and assessment process worth the increased data that they produce? How essential is it to ensure consistency at triage, to ensure that less apparent yet potentially serious conditions are detected, at the expense of making everyone wait longer to be triaged and assessed? Can well-looking patients with minor complaints safely wait for hours to be assessed by a physician without any formal initial enquiry or vital signs? Finally, what about the recommended outcomes for triage systems? Should formal triage and assessment systems incorporate more options than simply waiting to be treated in the emergency department (ED)?
Dug Andrusiek, from the School of Population and Public Health at the University of British Columbia, argues that formal ED triage tools are inefficient, unfair, and waste time and resources, followed by Michael Bullard, a professor in emergency medicine at the University of Alberta and leading member of the Canadian Triage Acuity Scale national working group (CTAS NWG), who responds that ED triage is required. Readers can follow the debate on Twitter and vote for either perspective, by going to @CJEMonline or by searching #CJEMdebate and #Triage.
For: Dug Andrusiek (@Andrusiek)
“Triage is simply the sorting out of patients to determine priority of need and proper placement.”
Since first being developed and used by Napoleon’s military surgeon, Baron Dominique Jean Larrey, triage, a system of resource allocation based on need rather than rank or social standing has become commonplace in emergency medical practice. While acknowledging that the modern ED is a world away from the 18th century battlefield, the basic goals of triage remain the same – in conditions of resource scarcity, sort out those seeking care to ensure that the highest priority is cared for first and that all patients are moved to the correct place for that care. The question is: Are formal triage systems that go beyond the basics of battlefield triage beneficial in the ED?
On the night of October 1, 2017, Stephen Paddock opened fire on a crowd gathered for the Route 91 Harvest Music Festival. Over the course of approximately 10 minutes, Paddock managed to hit over 600 people, and more than 500 of those gunshot victims arrived at Sunrise Hospital and Medical Center, the Level II Trauma Centre, the largest acute care facility in Las Vegas.Reference Staff 1 In an interview with Dr. Brian Goldman broadcast on the CBC’s “White Coat, Black Art,” attending emergency physician Dr. Kevin Menes estimated that he took 10 seconds to triage each patient.Reference Goldman 2 He did not use a complex computer algorithm or formalized triage algorithm, but rather a simple gestalt “Red, Orange, Yellow” system. After approximately 40 minutes of acting as the triage officer (a role he admits should rest with the most experienced physician), a backlog of patients requiring resuscitation occurred, and Dr. Menes handed triage over to a registered nurse, Deb Bowerman, with the simple instructions, as follows: “You saw what I’ve been doing. Put these people in the right places.”Reference Menes and Plaster 3
That night, Menes and his team treated about 200 patients, and only 16 died – all of this with a simple triage system that has been used in prehospital care and EDs for decades.
There are several other ways that Menes and his team could have sorted the patients arriving that night. They could have used the Manchester Triage System (MTS), Emergency Severity Index (ESI), or the closely related Australasian Triage Scale (ATS) or the CTAS.Reference FitzGerald 4 – Reference Beveridge 7 However, the scientific foundation for these systems is tenuous. A 2011 systematic review by Farrohknia et al.Reference Farrohknia, Castren and Ehrenberg 8 found insufficient, or lacking, evidence for the inter-rater reliability, and predictive validity seldomly evaluated, for the six formal triage systems included. The MTS demonstrated only fair predictive performance in a 2016 prospective study,Reference Steiner, Renetseder and Kutz 9 and the ESI under triages elder patients.Reference Grossmann, Zumbrunn and Frauchiger 10 Given the number of available options for ED triage, it is surprising that there is such a paucity of scientific support for their use. Perhaps part of the problem is that the triage systems are attempting to do more than just sort out patients and, in doing so, are trying to do too much.
A case in point is our own CTAS. Since first being introduced in 1998,Reference Beveridge 7 CTAS has become a staple in EDs around the country. Over that time, substantial effort has resulted in the introduction of a pediatric version, and five revisions. Those revisions now recur on a 4-year-cycle, much like the American Heart Association/International Liaison Committee on Resuscitation (AHA/ILCOR) Scientific review. Unlike the consensus updates issued by ILCOR and the AHA, CTAS revisions lack scientific evidence, basically because there is very little. Between 2012 and 2016 (the most recent 4-year review period), a total of only four related peer-reviewed articles had been indexed in PubMed (search term: “Canadian Triage Acuity Scale, CTAS, Validity”).
As noted, CTAS has become more than a sorting tool. According to the CTAS website, it enables examination of “patient care processes, workload, and resource requirement relative to case mix and community needs.” The CTAS literature goes further and explains how CTAS will help ED managers to 1) measure case mix (volume and acuity); 2) determine whether the ED has an operational plan and resources to meet patient needs; and 3) access the ED’s role within the hospital and healthcare region. Indeed, this is likely the real impetus behind the implementation and uptake of formal triage systems, including CTAS by hospitals. Also, herein lies the difficulty with formal triage systems like CTAS; they attempt to take on too much and miss the very basic objective of triage, which is to get the right patient to the right place during the right time. Any additional requirements for triage processes needlessly complicate and muddle that objective.
Let us examine these three administrative goals individually. The last goal (to access the ED’s role within the hospital and healthcare region) is opaque at best. The primary role of an ED is simply to treat acute emergency cases. Most of the CTAS, category 1 to 3, patients can be treated in an ED only. However, a proportion of level 5 cases certainly could be assessed and treated in a primary care physician’s office or walk-in clinic. It is unclear how enumerating the number of CTAS 5 cases that are seen in an ED will help influence decision-making regarding the number of primary care physicians or walk-in clinics in a given jurisdiction.
The second administrative goal is similarly dissociated and obliquely related to CTAS. There are far easier ways of knowing that an extra resuscitation bay is required, or that a first aid/fast-track area will improve flow-through in the ED than by reviewing the CTAS census for a given year. As with the triage system itself, the answer to the question – “What resources does the emergency department need?” – is generally tacitly known and easily solicited from those who work in the ED itself.
The first administrative goal, to measure case-mix, is perhaps the most difficult objective for formal triage systems, such as CTAS. Measuring case-mix or risk adjustmentReference Lezzoni 11 is incredibly difficult and relies on several key elements: outcome, time frame, population, and purpose. First purpose: If formal triage systems are to help with regional, hospital, and departmental planning, then the triage tool needs to reflect, by definition, some element of that purpose. For example, health authority planners may want to know more about the census of CTAS level 3 to 5 cases attending an ED while they are considering whether to build an new ED, urgent care facility, or walk-in clinic in a given area, because each of these facilities (and the attending patients) have different diagnostic and care needs. Yet, EDs attract notoriously heterogeneous patient populations, including psychiatric patients, making it difficult and almost impossible to devise valid and reliable scales. EDs also, by their very nature, look at a very short time horizon. Boarding, or crowding, is perhaps the biggest and most pressing issue for EDs across Canada and North America. Not much is added to the conversation by saying “We have had five CTAS 4 patients waiting for admission to the ward for over 72 hours,” that is not captured by saying, “We have had five patients who have waited over 72 hours for a bed on the ward.” Flow through the ED for CTAS 1 and 2 patients is rarely a problem, and, again, nothing is added by mentioning that the multi-trauma patient is CTAS level 1. Finally, and most importantly, case-mix, like all good healthcare, relies on having a well-defined outcome. This questions is perhaps the most difficult and vexing issue for any formally devised triage scale: Which outcome measure is most meaningful for the entire ED census? The problem of which outcome to use to evaluate and revise any formal triage system is simple on the left-hand side of the scale (levels 1 and 2) because any delay in diagnostic services and/or treatment will result in death. But can the same be said for all of the level 3 cases? Certainly, levels 4 and 5 cases that risk death are either misclassified or palliative.
So, we return to the wisdom of Dr. Menes who so sagely advised nurse Deb Bowerman: “Put them in the right place.” Also, we may want to add to not bother giving them a formal triage system score, be it MTS, ESI, ATS, or CTAS, because they take four times as long and offer no greater accuracy.Reference Curran-Sills and Franc 12
Against: Michael Bullard
“Emergency department triage is required.”
In a perfect world, ED capacity would equal demand, and there would be no delays in accessing appropriate care for all patients. The reality is that, in most urban, regional, and busy rural EDs, despite strong advocating by our emergency medicine leaders about the need to address system overcrowding, volumes continue to exceed available treatment spaces. Moreover, despite evidence to suggest that volumes are predictable, EDs are frequently faced with inadequate resources to manage peak demands.Reference Affleck, Parks and Drummond 13 , Reference Bullard, Villa-Roel and Bond 14 Although ED volume increases across Canada may have peaked, the acuity, complexity, and number of elderly ED patient presentations continue to rise here and elsewhere.Reference Rowe, Bond and Ospina 15 Using the Asplin input, throughput, output model, unless throughput and output can match input, waits for care will continue to occur.Reference Asplin, Magid and Rhodes 16
The majority of Canadian EDs have made remarkable efforts to reach the ideal state where all patients who arrive can be seen quickly. The addition of fast-track areas, intake areas, internal waiting rooms, and/or adoption of other innovative solutions has provided some benefits. Many EDs have undertaken Lean processes to identify strategies to improve patient flow. Although these projects often demonstrate flow improvements, these gains are difficult to sustain, particularly when they result in increased patient volumes or distribution shifts.Reference Rowe, Bond and Ospina 17 The only way to truly impact ED input and output is to determine why EDs are the default destination for a majority of system shortfalls and start investing in those capacity gaps.Reference Han, Ospina and Blitz 18 , Reference Krebs, Kirkland and Chetram 19 Only governments and system administrators can decide where best to invest where money and resources will do the most good. In the meantime, safely and efficiently prioritizing ED patients on arrival based on acuity, risk, and urgency is even more important in times of overcrowding.
Initially, triage was conducted as a subjective emergent, urgent, or non-urgent sorting of patients by nurses or registration personnel. In the 1990s, it was realized, both in Canada and internationally, that a more formal, reliable, and valid process was urgently needed. Much like emergency physicians apply various decision rules (e.g., Ottawa rules) to help support their clinical judgement, triage scales were developed to support nurse clinical decision-making and also to promote sensitivity over specificity. There are now four well-recognized 5-level triage scales in wide use internationally. They include the ATS, 4 MTS, 6 ESI, 5 and CTAS.Reference Beveridge 7 All four scales have shown good to excellent inter-rater reliability when using desktop case-based scenarios.
Since CTAS was first implemented in 1999, there have been nine studies in Canada evaluating CTAS inter-rater reliability demonstrating moderate to good inter-rater reliability in blinded or inter-observer studies further enhanced by computer decision support.Reference Worster, Sando and Fernandes 20 - Reference Dong, Bullard and Meurer 23 Further, six national and three international validity studies found excellent correlation between CTAS acuity admission rates and resource utilization.Reference Dong, Bullard and Meurer 24 – Reference Worster, Fernandes, Eva and Upadhye 27
Moreover, reflecting the growing global issue of overcrowding in EDs, through international agreements, CTAS has been adapted to support their needs by 11 countries (Taiwan, Japan, South Korea, Trinidad and Tobago, Barbados, Turks and Caicos, Costa Rica, Hungary, Saudi Arabia, Qatar, and Portugal). There have been six publications from Taiwan, Japan, and Saudi Arabia looking at post-implementation reliability and validity within their systems and able to replicate or improve on the results of our Canadian studies.Reference Nc, Yen and Tsai 28
Not all ED patients require a detailed and comprehensive triage. For example, patients with immediate life- or limb-threatening conditions are generally recognized by an initial critical first look and directed immediately to a resuscitation area. Clearly, triage should not prevent timely and appropriate care. Triage can, however, improve the accuracy of assessment and assignment of severity. The triage times reported in Alberta and Ontario studies, which noted median times of 2.5 and less than 5 minutes, respectively. In Japan, nurses found their mean triage times shortened from 2.9 to 1.9 minutes, and differences in urgency assigned by triage nurses and emergency physicians decreased from 34.2% to 12.2%.Reference Hamamoto, Yamase and Yamase 29
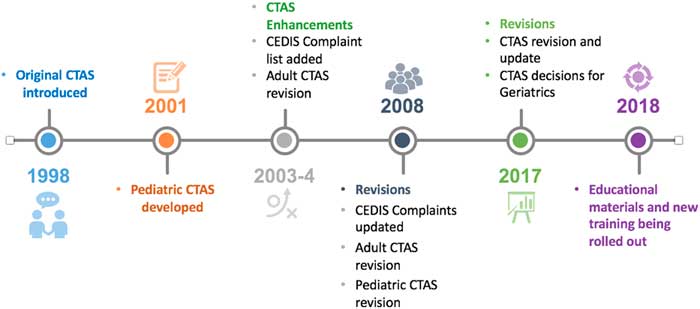
All triage scales define vital sign abnormalities to help identify patients needing immediate or emergent care, while also helping identify stable patients at lower risk. Since its introduction in 1998, triage needs have evolved. The CTAS has been adapting to meet the needs of Canadian clinicians and departments and revised and updated six times to address changes in care delivery and feedback from nurses, physicians, and the public. Additional features have been added to enhance sensitivity and positively impact patient safety (Figure 1). In 2001, Paediatric CTAS was developed, identifying the knowledge of physiological, anatomical, and developmental differences required to appropriately triage children (“children are not just small adults”). The nationally developed Canadian Emergency Department Information System (CEDIS) Presenting Complaint list was incorporated into the CTAS in 2004. Following the severe acute respiratory syndrome (SARS) epidemic in 2003, screening for communicable diseases and masking or isolating potentially contagious patients were added to the triage process to protect other patients and staff.

Figure 1 CTAS Timeline Graphic
Further revisions to CEDIS and both Paediatric and Adult CTAS occurred in 2008. The most recent 2016 CTAS update has focused on the challenges of appropriate triage decision-making for the growing population of elderly patients. All CTAS publications can be accessed at http://ctas-phctas.ca.
New training regarding elderly patients will focus on understanding the homeostatic changes that occur with advancing age, evaluating cognitive impairment, the impact of comorbid conditions and polypharmacy, and atypical presentations of common diseases.Reference Bullard, Melady and Emond 30 The most recent update also reflects a collaboration with the Society of Obstetrics and Gynaecologists of Canada where the CTAS NWG assisted them with the development of their Obstetrical Triage Acuity Scale, whereas a number of CTAS pregnancy-related special modifiers were updated to align with their scale.Reference Gratton, Bazaracai and Cameron 31 Finally, a CTAS 3 frailty modifier has been added for vulnerable patients at risk when they are subject to prolonged delays.Reference Bullard, Musgrave and Warren 32
CTAS was never designed for a mass casualty incident (MCI) situation, as described earlier by my colleague, especially one with the magnitude of the Harvest Music Festival shootings in Las Vegas. Because of nurse familiarity with CTAS, however, it has been used successfully in MCI simulations where the hospital resources are not as severely taxed. Recently, Alberta Health Services has introduced Rapid Assessment Triage for Emergency Department (RATE) as a 3-level triage tool to be used in the hospital, when normal resources are overwhelmed, rather than utilize Simple Triage and Rapid Assessment (START), which was designed specifically for prehospital use. This integrates with most hospital disaster plans with patients designated red (resuscitation/emergent), yellow (urgent) or green (less urgent/ambulatory) using CTAS critical look and vital sign severity definitions to limit the need for special training and can be applied in seconds.
Apart from its sorting function, triage has an important potential role to play within Canadian society. It should be recognized as a national disgrace that we have such rudimentary data regarding ED visits for inter-provincial, inter-hospital, and health outcomes comparisons. This is especially important for the vulnerable populations served in the ED (including socioeconomically disadvantaged, indigenous peoples [First Nation, Metis, and Inuit] and those with addictions). In today’s world, “data are power,” and without standardized collection and reporting of ED data, we continue to struggle to make our case for system change. Computer decision support can improve accuracy, an important consideration for jurisdictions using CTAS scores as part of their funding mechanism. Finally, the incorporation of artificial intelligence promises to assist clinicians with decisions in the future, and this requires accurate data from triage to discharge.
Prolonged waits for care in our Canadian EDs are not fair for anyone; however, the system’s capacity has been under strain for decades, especially at high volume, high acuity hospitals. Because large volumes, long patient waits, system overcrowding, and care gaps remain in most EDs in 2018, prioritizing ED patients as safely and efficiently as possible remains a compelling need. While resources allocated to triage remain a concern, trained triage nurses and paramedics have shown the greatest ability to accurately apply the CTAS while continuing to exercise their clinical judgement to override the tool when indicated. To support triage decision-making for the entire spectrum of ED presentations, the CTAS needs to be a granular tool. It can and should be applied within seconds to minutes, depending on patient acuity, by skilled health professionals. Until Canadian hospitals have the human and physical resources to be able to alleviate patients waiting 24 hours a day, 7 days a week, 365 days a year, sorting patients by urgency and streaming them to the most appropriate care space will remain a priority. Combining the objectivity of the CTAS and the clinical judgement and communication skills of experienced health professionals affords patients and emergency providers a valid and accurate level of safety.
Keywords: debate, emergency department, resources, triage
Competing interests: None declared.