INTRODUCTION
Acute myocardial infarction (MI) is diagnosed when the electrocardiogram (ECG) shows ST-segment elevation in at least two contiguous leads or new onset of a bundle branch block in combination with persistent chest discomfort (ST-segment elevation myocardial infarction; STEMI).Reference Roffi, Patrono, Collet, Mueller, Valgimigli and Andreotti1 In such cases, immediate cardiac catheterization is mandatory to prevent irreversible damage of the heart muscle. Early reperfusion therapy for patients with STEMI improves cardiovascular outcomes. However, some patients with acute MI present without symptoms or with symptoms other than chest pain.Reference Deedwania and Carbajal2 In a multinational, prospective, and observational study including 20,881 patients, 8.4% of patients with acute coronary syndromes did not have chest pain.Reference Brieger, Eagle, Goodman, Steg, Budaj and White3 These patients were frequently misdiagnosed and, therefore, undertreated. Those patients have increased hospital mortality rates.Reference Brieger, Eagle, Goodman, Steg, Budaj and White3 Patients presenting with syncope were at a higher risk of dying.
We report a case of a female patient with acute MI presenting with syncope and AV block without angina or typical ST-segment elevation.
CASE REPORT
An 86-year-old woman was admitted because of her first syncopal episode, without further symptoms. ECG at admission showed a high-degree AV block with a stable escape rhythm of 50 beats per minute, narrow QRS complexes, an isolated ST elevation in lead III, and an incomplete right bundle branch block (Figure 1). Echocardiography did not reveal any localized wall motion abnormalities and excluded valvular heart disease. There was no history of diabetes mellitus, and the glucose level at admission was within a normal range. Because of hypertension, the patient was on chronic treatment with a beta-blocker, an angiotensin II receptor antagonist, hydrochlorothiazide, and an aldosterone antagonist. The first blood test was unremarkable; the initial high-sensitive cardiac troponin I (hsTNI) level (Abbott ARCHITECT STAT high-sensitive troponin I immunoassay, Wiesbaden, Germany) was negative (7 pg/ml). The patient was scheduled for a pacemaker implantation. A second blood test of biomarkers three hours later showed a marked elevation of hsTNI (25,290 pg/ml). Immediate cardiac catheterization was performed revealing subtotal ostial stenosis of the right coronary artery (Figure 2A). The left coronary artery had no significant stenosis (Figure 2B and 2C). Stent implantation was performed successfully (Figure 2D). During the hospital stay, the patient remained asymptomatic, and the AV block disappeared (Figure 3). Five days later the patient could be discharged without further sequelae.
Figure 1. Twelve-lead ECG. ECG at admission with a high-degree AV block and stable escape rhythm of 50 beats per minute, with narrow QRS complexes, an isolated ST elevation in lead III, and an incomplete right bundle brunch block.
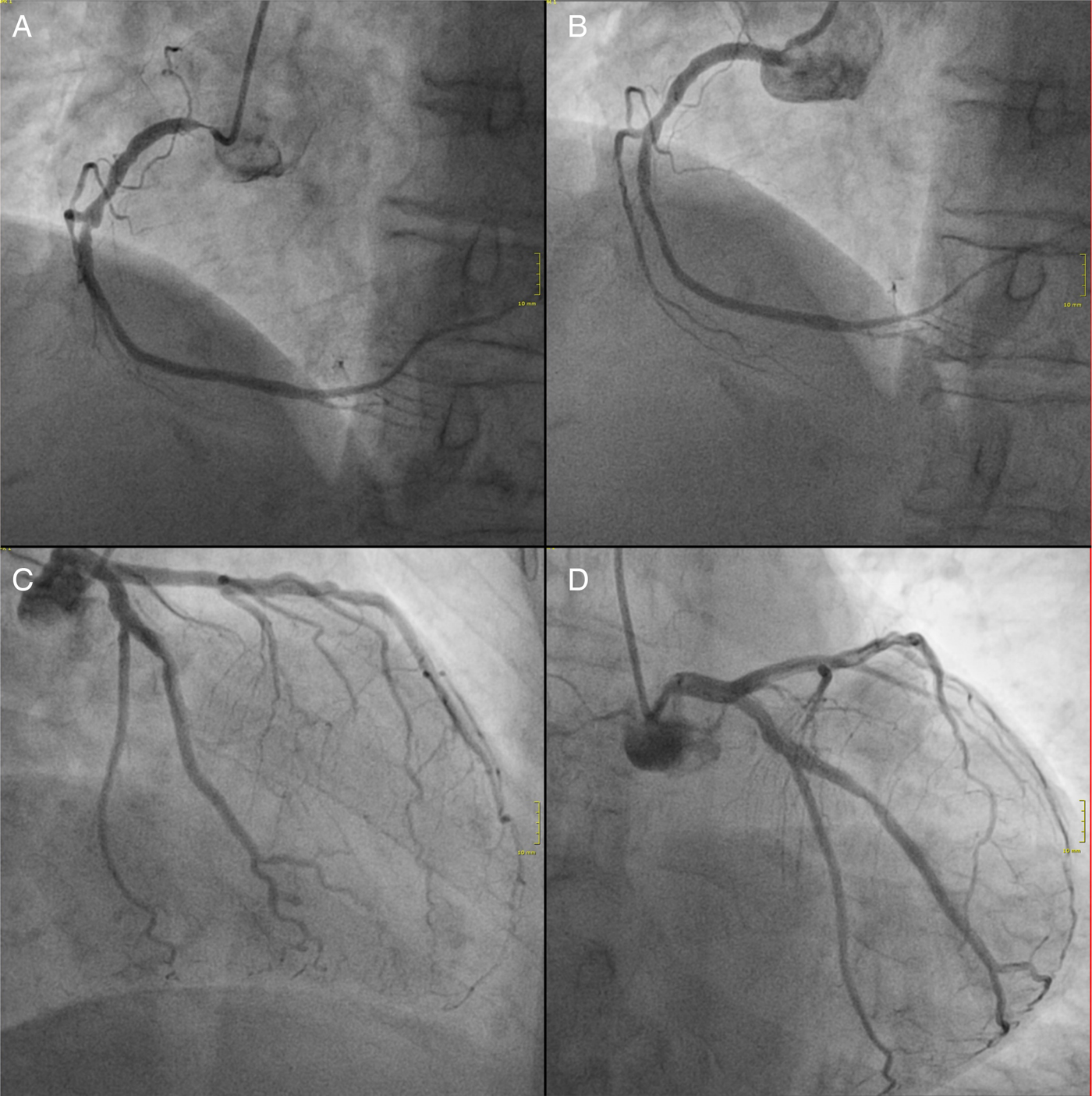
Figure 2. Coronary angiography. (A) Subtotal ostial occlusion of the right coronary artery (40°/0° projection). (B) Right coronary artery after successful ostial stent deployment. (C and D) Left coronary artery without significant stenosis in two projections (C in −30/0° projection; D in 0°/−30° projection).
Figure 3. Twelve-lead ECG. ECG at discharge with a sinus rhythm, without an AV block.
DISCUSSION
Current guidelines recommend permanent pacing in patients with an acquired second-degree Mobitz type II and high-degree AV block, regardless of symptoms.Reference Kusumoto, Schoenfeld, Barrett, Edgerton, Ellenbogen and Gold4 In patients with a newly identified AV block, transthoracic echocardiography should be performed to exclude apparent structural heart disease.Reference Kusumoto, Schoenfeld, Barrett, Edgerton, Ellenbogen and Gold4 Furthermore, laboratory testing including thyroid function tests, potassium, and pH level is recommended. There is no recommendation for routine measurement of the hsTNI level. However, elderly female patients are at a high risk of a silent MI.Reference Cho, Jeong, Ahn, Kim, Chae and Kim5 It has been shown that painless MI was associated with more adverse events than painful MI because of treatment delay leading to a higher total ischemic burden.Reference Pek, Loy, Wah, Ho, Zheng and Fook-Chong6 In conclusion, especially in the emergency department (ED), we should consider silent MI in all high-risk patients. Measurement of hsTNI in such high-risk groups is a simple tool that might help to improve diagnostic and treatment efficiency. Immediate adequate treatment, in our case, stenting of the right coronary artery as the target lesion, prevents inappropriate therapy. In this patient, unnecessary pacemaker implantation was prevented, and the prognosis of this patient might have been improved.
Acknowledgements
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Competing interests
The authors have no conflicts of interest to declare.





