The term cardiometabolic risk was proposed by the American Diabetes Association and the American Heart Association, and it is used to describe a set of clinical signs, such as dyslipidaemias, insulin resistance, obesity and high blood pressure(Reference Moschonis, Tsoutsoulopoulou and Efstathopoulou1,Reference Eckel, Kahn and Robertson2) . These metabolic changes are related to chronic non-communicable diseases, which have been diagnosed early in childhood and adolescence(Reference Hobbs, Pearson and Foster3,Reference Agirbasli, Tanrikulu and Berenson4) .
In adolescence, epidemiological studies have shown an association between unhealthy eating behaviours, such as skipping meals, especially breakfast, and increased cardiometabolic risk(Reference Hallström, Labayen and Ruiz5–Reference St-Onge, Ard and Baskin7).
Breakfast skipping among adolescents has ranged from 1·3 to 74·7 % worldwide(Reference Monzani, Rapa and Fuiano8). In general, skipping this meal has been associated with excess body weight and abdominal obesity(Reference Forkert, De Moraes and Carvalho9), increased blood pressure(Reference Cayres, Júnior and Barbosa10), deleterious effects on lipid profile(Reference Ibáñez and Fernández-Alvira11) and glycidic profile(Reference Jakubowicz, Wainstein and Ahren12,Reference Jakubowicz, Waintein and Zohar13) . The mechanisms that might explain the relationship between breakfast skipping and metabolic outcomes are related to a possible high energy intake after the long fasting period(Reference Kim, Song and Park14), fasting-induced insulin resistance(Reference Smith, Gall and McNaughton15), appetite regulation(Reference Pereira, Erickson and McKee16), changes in glycaemic homoeostasis and interruption of gene expression of circadian cycles involved in glucose metabolism(Reference Jakubowicz, Waintein and Zohar13).
As far as is known, no nationwide representative study has investigated the association between breakfast skipping and cardiometabolic risk factors in Brazil. Thus, considering the importance of regular breakfast consumption for adolescents’ health and that the breakfast skipping habits during adolescence may persist into adulthood which can have deleterious effects on metabolic outcomes, the objective of the present study was to estimate the prevalence of breakfast skipping and its association with cardiometabolic risk factors in Brazilian adolescents.
Methods
Study design and data sources
This is an analysis of data from the Study of Cardiovascular Risks in Adolescents (ERICA – Estudo de Riscos Cardiovasculares em Adolescentes). ERICA is a school-based, cross-sectional study aiming to estimate the prevalence of diabetes mellitus, obesity and cardiovascular risk factors in addition to insulin resistance and inflammatory markers, which examined a nationwide representative sample of 12–17-year-old adolescents enrolled in public and private schools in Brazilian cities with more than 100 thousand inhabitants(Reference Vasconcellos, Silva and Szklo17).
The research population was stratified into thirty-two strata, consisting of twenty-seven capitals and five sets of municipalities with more than 100 thousand inhabitants in each of the five geographical regions of the country(Reference Bloch, Szhlo and Kuschnir18). For each geographic stratum, schools were selected with probability proportional to the size and inversely proportional to the distance from the capital. Thus, the sample is representative for the set of medium- and large-sized cities (>100 thousand inhabitants) at national and regional levels and for the Brazilian capitals and the Federal District. In addition, the location of the school (urban or rural area) and the type of administration (public or private) were considered, allowing the concentration of the sample around the capitals, which reduced costs and facilitated the logistics of the research project, especially as regards collection of blood samples and adequacy of pre-analytical procedures. In total, 1247 schools (out of 1251 selected ones) were evaluated in 122 municipalities (out of 124). More details on the sampling process can be found in the study of Vasconcellos et al.(Reference Vasconcellos, Silva and Szklo17).
In the second sampling stage, three classes from each school were selected, considering combinations of shift (morning and afternoon) and eligible years (seventh, eighth and ninth year of elementary school and first, second and third year of high school). In the third stage, in each combination of shift and year, a class was selected, and all students in the respective class were invited to participate in ERICA(Reference Vasconcellos, Silva and Szklo17,Reference Bloch, Szhlo and Kuschnir18) . Because of the need for 12 h of fasting, only students on the morning shift participated in blood collection (Fig. 1).
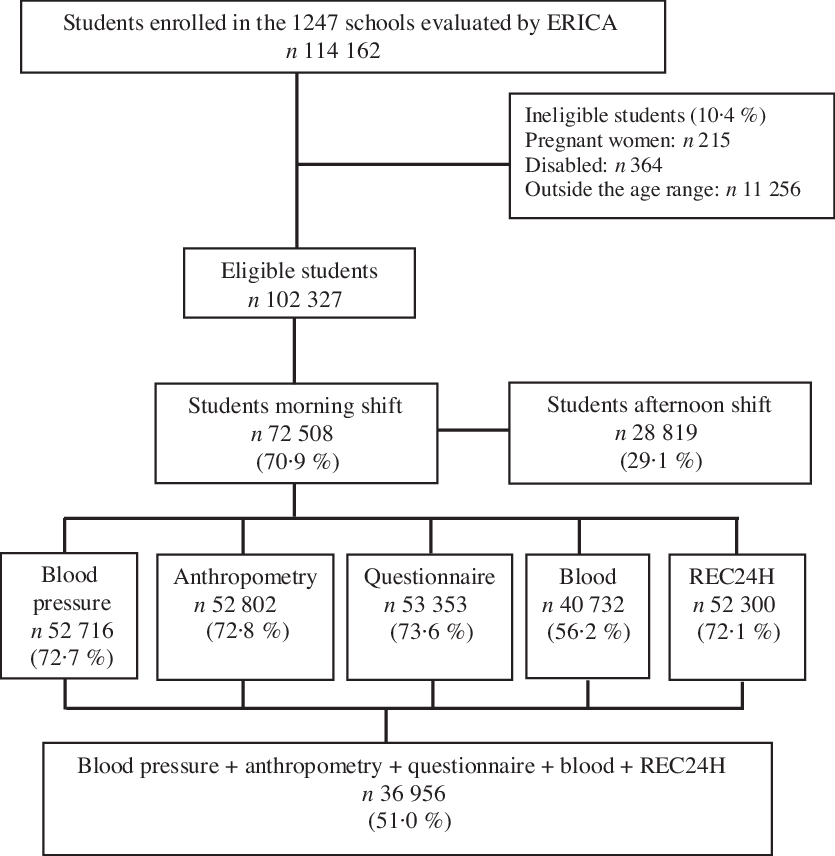
Fig. 1. Flowchart of eligible adolescents from the Adolescent Cardiovascular Risk Study (ERICA), Brazil, 2013–2014. REC24H, 24-h recall.
The students of the selected classes who signed the consent form and presented the Free and Informed Consent Term signed by their parents or guardians were interviewed and examined. Adolescents who did not belong to the age group of 12–17 years old, pregnant adolescents and individuals with temporary or permanent physical or mental disabilities were not eligible for the study.
ERICA was conducted according to the principles of the Declaration of Helsinki. The study was approved by the Committee for Ethics in Research of the Institute of Collective Health Studies, Federal University of Rio de Janeiro (Process 45/2008) and of each one of the twenty-six states and the Federal District. Permission to conduct the study was obtained in all State and local Departments of Education and in all schools. The privacy and information confidentiality of students was guaranteed.
Data collection instruments and procedures
Data collection took place between March 2013 and December 2014 and was performed by a team of previously trained evaluators, using standardised techniques to ensure the students’ privacy. The questionnaire was self-administered and applied using an electronic data collector, a Personal Digital Assistant (model LG GM750Q). This instrument contained about 100 questions distributed into eleven blocks: socio-demographic aspects, occupational activities, physical activity, eating behaviour, smoking, alcohol consumption, reproductive health, oral health, referred morbidity, sleep duration and common mental disorders(Reference Bloch, Szhlo and Kuschnir18).
Breakfast skipping
Breakfast skipping was assessed using the question ‘Do you have breakfast?’, with the following answer options: ‘I don’t have breakfast’, ‘I have breakfast sometimes’, ‘I have breakfast almost every day’ and ‘I have breakfast every day’. Breakfast skipping was estimated from the combination of the categories: ‘I don’t have breakfast’, ‘I have breakfast sometimes’ and ‘I have breakfast almost every day’.
Cardiometabolic risk factors
Weight and height measurements were used to calculate the BMI (weight/height2). Weight status was assessed using age- and sex-specific BMI z-scores according to the WHO’s curves. Adolescents with BMI z-score ≥ +1 were classified as excess body weight(19).
Weight was defined by a single measurement on a Líder® P150m electronic scale with 200 kg capacity and 50 g weight change detection. Height was determined by the average of two measurements taken sequentially (a maximum variation of 0·5 cm between the two measurements was accepted), using a Alturexata® portable calibrated and dismountable stadiometer with resolution in millimeter and field of view use of up to 213 cm(Reference Bloch, Szhlo and Kuschnir18,Reference Silva, Klein and Souza20) . The specific procedures for each measure are described in detail in Bloch et al.(Reference Bloch, Szhlo and Kuschnir18).
Waist circumference was measured with a Sanny® anthropometric glass fibre tape, with resolution of 1 mm and length of 1·5 m. Waist circumference was considered high when ≥the 90th percentile for adolescents under 16 years(Reference Fernández, Redden and Pietrobelli21) and ≥90 cm for boys and ≥80 cm for girls for adolescents ≥16 years(Reference Alberti, Zimmet and Shaw22). The waist:height ratio was determined by measuring waist circumference (cm) and height (cm), and values ≥0·5 cm were considered as risk(Reference Ashwell and Hsieh23).
For blood collection, a standardised research protocol was used and applied in the twenty-seven centres. All the biochemical analyses of the study were performed in a single reference laboratory, with strict quality control, supported by the local partner laboratories that managed the collection and receipt of the samples, allowing standardisation of measures and uniformity of results. The laboratories received documentation with a protocol to be followed at all stages, from scheduling to transportation to the central unit, and the labelled kit for collecting blood from each adolescent. The adolescents were instructed to fast for 12 h before collection. A questionnaire was applied before the exam to confirm compliance with fasting(Reference Faria-Neto, Bento and Baena24).
Fasting blood samples were collected for analyses of glucose, insulin, lipid profile (total cholesterol (TC), HDL-cholesterol and TAG) and glycated Hb(HbA1c). Cholesterol associated with LDL-cholesterol was calculated using the Friedewald formula(Reference Xavier, Izar and Faria Neto25). The presence of high levels of blood glucose, insulin, HbA1c, TC, TAG and LDL-cholesterol and low levels of HDL-cholesterol was considered as inappropriate. Table 1 presents the cut-off points adopted. A full description of the ERICA methods can be found in Bloch et al.(Reference Bloch, Szhlo and Kuschnir18)
Table 1. Cut-off points used for blood testing results: ERICA, Brazil, 2013–2014
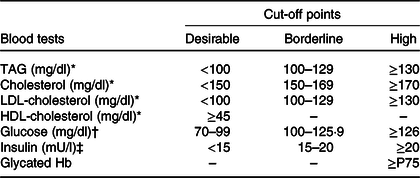
ERICA, Study of Cardiovascular Risks in Adolescents; P75, 75th percentile of population distribution.
* V Brazilian Guidelines on Dyslipidaemias and Prevention of Atherosclerosis(Reference Xavier, Izar and Faria Neto25).
† Diagnosis and Classification of Diabetes Mellitus(26).
‡ I Guidelines of Prevention of Atherosclerosis in Childhood and Adolescence(Reference Back Giuliano, Caramelli and Pellanda27).
Covariables analysed
The covariables analysed in the present study were sex (male and female), age (categorised into age groups: 12–14 and 15–17 years), sexual maturation stage (the latest Tanner stages among male and female students), type of school attended (according to type of administration, public or private, as a proxy for socio-economic status(Reference Moraes, Moreira and Oliveira28,Reference Moreira, Sichieri and Reichenheim29) , energy consumption (in kcal), estimated from data collected by applying a 24-h dietary recall(Reference Barufaldi, Abreu and Veiga30) and behaviours related to lifestyle, namely physical activity (adolescents who did not practise any type of activity were considered to be inactive; those who practised <300 min/week were considered as insufficiently active and those who practised ≥300 min/week were considered to be active)(31), screen time (h/d) considering the following categories: ≤2, 3–5 and ≥6 h/d(Reference Cureau, Ekelund and Bloch32), alcohol consumption (drinking at least one dose of alcohol in the last 30 d(Reference Coutinho, França-Santos and Magliano33) and smoking (use of cigarettes at least one day in the last 30 d)(Reference Warren, Jones and Peruga34). These covariates were analysed because they are observed in the literature as potential confounding factors in the association between breakfast skipping and cardiometabolic factors(Reference Smith, Gall and McNaughton15,Reference Alexander, Ventura and Spruijt-Metz35–Reference Mustafa, Majid and Zoi38) .
Statistical analysis
Statistical analyses were performed using the software Stata (Statistical Software for Professionals), version 12.0. The survey (svy) module was used to consider the weight of the sample and the research design.
Prevalence of breakfast skipping (% with the respective 95 % CI) and its association with the covariates (sex, age, Tanner stage, energy consumption, type of school attended, physical activity, screen time, alcohol consumption and smoking) were assessed using the χ 2 test with the second-order Rao-Scott correction, adopting a significance level of 5 %.
The association between breakfast skipping and each outcome of interest was estimated by Poisson regression models, obtaining the crude and adjusted prevalence ratios (PR) with 95 % CI. In the adjusted analysis, we used all analysed covariates and the least informative covariates were successively removed from the model in a backward stepwise elimination based on the Akaike information criterion.
Results
In the present study, 36 956 adolescents were evaluated, 50·2 % of whom were females; 53·4 % were between 15 and 17 years old; 77·7 % studied in public schools; 45·2 % were considered as physically active; 20·5 % had screen time ≥6 h/d, 22·5 % consumed alcoholic beverages, 4·4 % were classified as smokers and average energy consumption was 9623 kJ/d (2300 kcal/d) (Table 2).
Table 2. Prevalence of skipping breakfast, according to socio-demographic and economic variables, stage of sexual maturation, energy consumption and lifestyle of adolescents (n 36 956), ERICA, Brazil, 2013–2014*
(Percentages and 95 % confidence intervals)
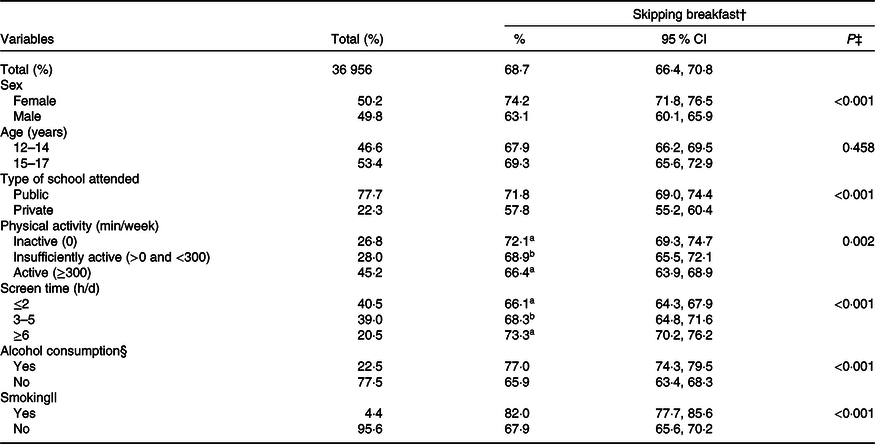
ERICA, Study of Cardiovascular Risks in Adolescents.
a,b Values within a column with unlike superscript letters were significantly different.
* Missing: screen time = 3056, alcohol consumption = 1217 and smoking = 221.
† Skipping breakfast: daily non-consumption.
‡ P value associated with the χ 2 test.
§ Ingestion of at least one dose of alcohol in the last 30 d.
|| Cigarette use at least 1 d in the last 30 d.
Prevalence of breakfast skipping was 68·7 %; it was significantly higher among girls (74·2 %), students from public schools (71·8 %), inactive adolescents (72·1 %), with screen time ≥6 h/d (73·3 %), alcohol drinkers (77·0 %) and smokers (82·0 %), compared, respectively, with boys (63·1 %), private school students (57·8 %), active adolescents (66·4 %), with screen time ≤2 h/d (66·1 %), non-alcohol drinkers (65·9 %) and non-smokers (67·9 %) (Table 2).
Breakfast skipping, excess body weight and central obesity
Higher prevalence of excess body weight (PR = 1·30 (95 % CI 1·18, 1·43)) and central obesity, both considering WC (PR = 1·27 (95 % CI 1·01, 1·61)) as for the waist:height ratio (PR = 1·32 (95 % CI 1·13, 1·54)), was found in adolescents who skipped breakfast (Table 3).
Table 3. Prevalence and prevalence ratios of skipping breakfast, according to anthropometric characteristics, ERICA, Brazil, 2013–2014†
(Percentages and 95 % confidence intervals)
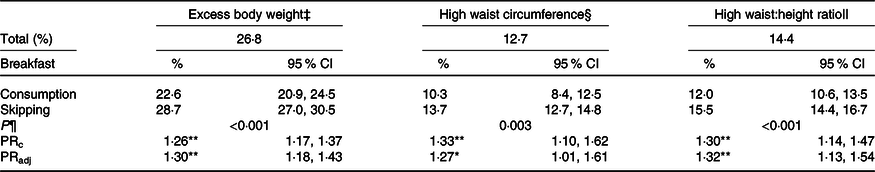
ERICA, Study of Cardiovascular Risks in Adolescents; PRc, crude prevalence ratio; PRadj, prevalence ratio adjusted for: sex, age, Tanner stage, type of school attended, physical activity, screen time, alcohol consumption, smoking and total energy consumption.
* P < 0·05, ** P < 0·01.
† PRc and PRadj considering consumption as reference category.
‡ ≥+1 z-score(19).
§ ≥90th percentile for adolescents under 16 years of age(Reference Fernández, Redden and Pietrobelli21) and ≥80·0 cm for girls and ≥90·0 cm for boys for adolescents ≥16 years old(Reference Alberti, Zimmet and Shaw22).
|| ≥0·50 cm(Reference Ashwell and Hsieh23).
¶ P value associated with the χ 2 test.
Breakfast skipping and lipid and glycidic profiles
Table 4 shows that, for lipid profile, there was a significant association, after adjustment, between breakfast skipping and TC; adolescents who skipped breakfast had 14 % more prevalence of high TC than those who had breakfast every day.
Table 4. Prevalence and prevalence ratios of skipping breakfast, according to the biochemical characteristics of the adolescents, ERICA, Brazil, 2013–2014†
(Percentages and 95 % confidence intervals)
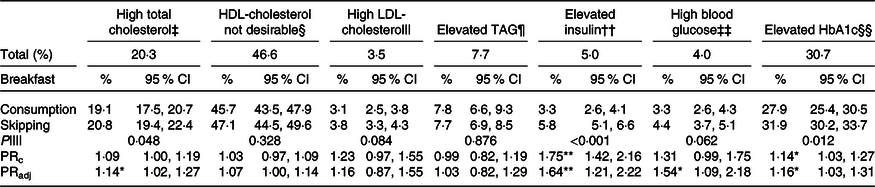
ERICA, Study of Cardiovascular Risks in Adolescents; HbA1c, glycated Hb; PRc, crude prevalence ratio; PRadj, prevalence ratio adjusted for: sex, age, Tanner stage, type of school attended, physical activity, screen time, alcohol consumption, smoking and total energy consumption; P75, 75th percentile of population distribution.
* P < 0·05, ** P < 0·01.
† PRc and PRadj considering consumption as reference category. Missing: total cholesterol = 105, HDL-cholesterol = 105, LDL-cholesterol = 119, TAG = 107, insulin = 143, glycaemia = 160, HbA1c = 53.
‡ ≥170 mg/dl(Reference Xavier, Izar and Faria Neto25).
§ <45 mg/dl(Reference Xavier, Izar and Faria Neto25).
|| ≥130 mg/dl(Reference Xavier, Izar and Faria Neto25).
¶ ≥130 mg/dl(Reference Xavier, Izar and Faria Neto25).
†† ≥20 mU/l(Reference Barufaldi, Abreu and Veiga30).
‡‡ ≥100 mg/dl(Reference Back Giuliano, Caramelli and Pellanda27).
§§ ≥P75.
|||| P value associated with the χ 2 test.
In addition, there was higher prevalence of high insulin levels among adolescents who skipped breakfast compared with those who did not (5·8 v. 3·3 %, P < 0·001), and the same result was found for HbA1c (31·9 v. 27·9 %, P = 0·012). In the adjusted analysis, breakfast skipping was associated with all variables of the glycidic profile. Adolescents who skipped breakfast had 64 % more prevalence of high insulin, 54 % more prevalence of high blood glucose and 16 % more prevalence of high HbA1c compared with adolescents who consumed this meal (Table 4).
Discussion
In ERICA, which was conducted with a representative sample of Brazilian adolescents, there was a high frequency of breakfast skipping. The prevalence of cardiometabolic risk factors was higher among adolescents who skipped breakfast, for example, excess body weight, central obesity and high levels of TC, fasting insulin, fasting glycaemia and HbA1c.
Among the studies that considered breakfast skipping among adolescents as non-daily breakfast consumption, the breakfast skipping prevalence was 37·6 % in Turkey(Reference Gokler, Bugrul and Metintas39) and 47·5 % among adolescents in a Brazilian city(Reference Cayres, Urban and Fernandes36).
Adolescents who skipped breakfast had higher prevalence of excess body weight and central obesity. Similar results were found in studies with adolescents from North America(Reference Deshmukh-Taskar, Radcliffe and Liu40,Reference Wang, Schwartz and Shebl41) , Egypt(Reference Talat and El Shahat42), Asia(Reference Khan, Khan and Burton43), Brazil(Reference Cayres, Urban and Fernandes36), as well as in a multicentre study with European and Brazilian adolescents(Reference Forkert, De Moraes and Carvalho9).
In the Healthy Lifestyle in Europe by Nutrition in Adolescence (HELENA) Study, Hallström et al.(Reference Hallström, Labayen and Ruiz5) found that male adolescents who skipped breakfast had higher rates of BMI, waist circumference and skinfold thickness, as well as higher levels of LDL-cholesterol, fasting insulin, fasting glucose and insulin resistance, while girls showed higher levels of skinfold thickness, BMI, fasting insulin and insulin resistance.
Longitudinal studies support the associations observed between breakfast skipping and excess body weight. Wang et al.(Reference Wang, Schwartz and Shebl41), in study with adolescents from New Haven and 4-year follow-up, considering breakfast skipping was defined as consuming breakfast 0–3 times a week, found that adolescents who skipped breakfast were 2·66 times more likely to be overweight and obese than those who had this meal.
Similarly, in the Childhood Determinants of Adult Health study, breakfast skipping in childhood was defined as not eating anything before going to school and in adulthood as not eating between 06.00 and 09.00 hours in the previous day, it was found that the habit of skipping breakfast in childhood tended to continue until adulthood and was associated with increased waist circumference, and with higher values of fasting insulin, insulin resistance and BMI, as well as higher concentrations of TC and LDL-cholesterol fraction(Reference Smith, Gall and McNaughton15).
This association between breakfast skipping and excess body weight can be explained by appetite regulation mechanisms, since not having breakfast can lead to less post-meal energy expenditure and contribute to changes in lipid and glucose metabolism(Reference Pereira, Erickson and McKee16). Thus, adolescents who skip breakfast stay on an empty stomach for a longer time, increasing ghrelin secretion, which leads to increased appetite and hyperphagia throughout the day. As a consequence, weight gain and body fat accumulation are increased(Reference Ibáñez and Fernández-Alvira11,Reference Pereira, Erickson and McKee16) . It is noteworthy that, in the present study, this association was maintained even after adjustments for total energy intake.
Concerning to lipid profiles, breakfast skipping was associated only with higher levels of TC. This result was different from the one found by Cayres et al.(Reference Cayres, Júnior and Barbosa10) and Silva et al.(Reference Silva, Padez and Sartorelli37) in Brazilian adolescents. Neither of them found an association between breakfast skipping and lipid profile markers (TC, HDL-cholesterol, LDL-cholesterol and TAG). On the other hand, results similar to those in the present study were found by Mustafa et al.(Reference Mustafa, Majid and Zoi38) While evaluating Malaysian adolescents, they found that those who never ate breakfast had higher levels of TC and LDL-cholesterol. Among adolescents of both sexes aged 10–18 years and living in Iran(Reference Shafiee, Kelishadi and Qorbani44) and Korean girls of the same age group(Reference Kim, Song and Park14), it was found that breakfast skipping was associated with greater likelihood of hypertriacylglycerolaemia.
Longitudinal studies indicate that the main factors that may explain the association between breakfast skipping and dyslipidaemia are increased appetite and high energy intake after the fasting period(Reference Kim, Song and Park14) and greater intake of saturated fat among adolescents who skip breakfast(Reference Smith, Gall and McNaughton15). Also, fasting-induced insulin resistance increases liver lipase activity(Reference Kim, Song and Park14) and stimulates higher concentrations of hydroxy methyl glutaryl Co-A reductase, which results in higher concentrations of cholesterol(Reference Smith, Gall and McNaughton15).
Unlike the findings of other observational studies, adolescents who skipped breakfast in ERICA had higher prevalence of high levels of fasting insulin, fasting glycaemia and HbA1c compared with adolescents who consumed this meal. Studies with Brazilian(Reference Silva, Padez and Sartorelli37), Malaysian(Reference Mustafa, Majid and Zoi38), Iranian(Reference Shafiee, Kelishadi and Qorbani44) and American(Reference Alexander, Ventura and Spruijt-Metz35) adolescents found no significant association between breakfast skipping and glucose profile.
Changes in the glycidic profile were found among young people in controlled, randomised and repeated measures clinical trials: breakfast skipping was associated with an increase in the mean 24-h blood glucose, even without changes in the 24-h energy expenditure, in lipid oxidation and thermal effect of food. These results indicating that changes in glycaemic homoeostasis precede some effect on energy balance(Reference Kobayashi, Ogata and Omi45,Reference Ogata, Kayaba and Tanaka46) .
Breakfast skipping may be associated with changes in the glycidic profile because prolonged fasting affects glycaemic homoeostasis, which results in decreased insulin and C peptide secretion and reduced glucagon peptide-1 responses(Reference Jakubowicz, Waintein and Zohar13). In addition, the absence of increased glucose levels as a result of fasting can decrease response capacity and memory of pancreatic β cells, leading to a reduction and delay in their response to insulin(Reference Jakubowicz, Wainstein and Ahren12).
In addition, some studies have linked breakfast skipping to interruption of gene expression in circadian cycles involved in glucose metabolism(Reference Jakubowicz, Waintein and Zohar13,Reference Ruddick-Collins, Johnston and Morgan47) . These genes respond to the content and timing of meals, which leads to a coordinated regulation of digestive and absorptive functions, as well as hormonal secretion, thereby preventing metabolic dysregulation during consumption of breakfast(Reference Froy48).
Although breakfast composition was not evaluated in the present study, it had a protective effect on glucose metabolism. Consumption of foods rich in protein and fibre, such as high-fibre cereals, whole grains, fruits and dairy products, contributes to reducing gastric emptying time, glucose digestion and absorption, as well as improving glycaemic control(Reference Silva, Padez and Sartorelli37,Reference Deshmukh-Taskar, Radcliffe and Liu40) .
Furthermore, breakfast consumption is associated with better diet quality(Reference Deshmukh-Taskar, Radcliffe and Liu40), healthier lifestyle(Reference Tambalis, Panagiotakos and Psarra49) as well as cognitive aspects related to improving school performance and memory(Reference Sampasa-Kanyinga and Hamilton50) and has been observed as a protective factor for obesity and general health(Reference Szajewska and Ruszczynski51), providing several benefits in bone and cardiovascular health(Reference Sandercock, Voss and Dye52,Reference Hunty, Gibson and Ashwell53) .
The cross-sectional design of the present study does not allow inferring causal relationships between breakfast skipping and presence of cardiometabolic risk factors, especially related to excess body weight, because adolescents with excess body weight can skip meals to lose weight(Reference Timlin, Pereira and Story54,Reference Hassan, Cunha and da Veiga55) . However, longitudinal studies have also found similar associations(Reference Kim, Song and Park14,Reference Smith, Gall and McNaughton15,Reference Wang, Schwartz and Shebl41) , supporting the results found among adolescents participating in ERICA.
The definition and variations in the cut-off points used by the studies to classify the habit of breakfast skipping can influence the results and their interpretation(Reference St-Onge, Ard and Baskin7). For example, Khan et al.(Reference Khan, Khan and Burton43), when evaluating adolescents from Bangladesh, defined skipping as not eating breakfast between 0 and 4 d/week and found a prevalence of 23 %. Among Brazilian adolescents, Hassan et al.(Reference Hassan, Cunha and da Veiga55) also found that prevalence depends on how breakfast skipping was defined and categorised. They noted that the prevalence of breakfast skipping ranged from 3·6 %, when the reference period was the previous week, to 39 %, when asked if the adolescent had eaten some solid food in the morning of the interview.
Thus, there is no clear definition or standardised categorisation of breakfast skipping among the different studies, which makes it difficult to compare their findings. The American Heart Association recently proposed definitions to improve and standardise the assessment of consumption and skipping of meals: food consumption occasions were defined as any episode that provides at least 210 kJ with 15 min of time elapsed between separate occasions. The distinction between meals and snacks should be at the discretion of the research participant, thus encompassing different social norms and cultural behaviours(Reference St-Onge, Ard and Baskin7).
In the present study, we chose to consider the answers ‘I don’t have breakfast’, ‘I have breakfast sometimes’ and ‘I have breakfast almost every day’ as skipping and to consider consumption only for adolescents who marked the option ‘I have breakfast every day’. It should be noted that the dietary guidelines for the Brazilian population(56) consider breakfast to be one of the three main meals of the day and recommend the daily consumption of this meal, this is why we chose to consider breakfast skipping as not having breakfast in a regular daily basis. Similar categorisations for breakfast skipping were used in previous studies(Reference Cayres, Urban and Fernandes36,Reference Gokler, Bugrul and Metintas39) .
The questionnaire used in the present study was self-administered and can be considered a possible limitation, as it depended on the adolescent’s memory and motivation to answer it. However, this type of questionnaire has been applied in other epidemiological researches conducted with students and it is considered an acceptable method for data collection(Reference Khan, Khan and Burton43,Reference Timlin, Pereira and Story54,Reference Hassan, Cunha and da Veiga55) . Other limitations that can be considered were the lack of information on other potential confounders which were not evaluated in the present study, for example, family income and race/skin colour. Family income has been associated with breakfast skipping and cardiometabolic outcomes in adolescents(Reference Smith, Gall and McNaughton15,Reference Hassan, Cunha and da Veiga55) ; likewise other studies with Brazilian adolescents(Reference Moraes, Moreira and Oliveira28,Reference Moreira, Sichieri and Reichenheim29) , in the present study, the type of school was considered as a proxy of the adolescents’ socio-economic level. Regarding race/skin colour, although some studies in the literature have used race/ethnicity as a confounding factor(Reference Wang, Schwartz and Shebl41,Reference Timlin, Pereira and Story54) in the relationship between breakfast skipping and weight status, Hassan et al.(Reference Hassan, Cunha and da Veiga55) found no significant association between skin colour and breakfast skipping among Brazilian adolescents.
The main strength of the present study is the school-based probabilistic sample with regional and national representativeness, which provides further insights into the association of food consumption and cardiovascular risk factor profile in adolescents(Reference Vasconcellos, Silva and Szklo17,Reference Bloch, Szhlo and Kuschnir18) . In addition, careful handling of information (training of evaluators for data collection, pilot testing for adequacy of questionnaires and standardised techniques) and use of standardised protocols minimise measurement errors. The wide range of demographic, socio-economic, sexual maturation, energy consumption and lifestyle-related data enabled the assessment of the association between breakfast skipping and multiple cardiometabolic risk markers; therefore, potential confounding factors could be controlled.
Conclusion
Breakfast skipping was very frequent among the studied adolescents, especially in females and public-school students. Adolescents who skipped this meal were more likely to have total and central obesity, as well as high levels of TC, fasting insulin, fasting glycaemia and HbA1c, regardless of lifestyle, sexual maturation, energy consumption, and demographic and socio-economic characteristics. Thus, breakfast skipping can be a harmful habit for adolescents’ cardiovascular health.
The present study highlights the importance of encouraging daily consumption of breakfast. In this context, the school environment is an ideal space for the promotion of healthy eating habits, supporting the implementation of nutrition education activities that aim to encourage adolescents to eat breakfast daily and choosing healthy food options for this meal.
Acknowledgements
The authors would like to thank the financial support provided by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil, through a master’s grant (M. R. S.; finance code 001). However, CAPES had no role in the design, analysis or writing of this paper.
M. R. S. contributed to the conceptualisation of the study, formal analysis, writing the original draft, and final review. M. E. A. N. contributed to formal analysis, interpretation of the findings, and writing the original draft. A. M. S. and A. P. M. contributed to the conceptualisation of the study, formal analysis, and final review. R. A. P. and M. G. F. contributed to formal analysis, review and editing and supervision. P. R. M. R. contributed to the conceptualisation of the study, formal analysis, writing the original draft, review and editing and supervision. All authors read and approved the final version of the manuscript.
The authors declare that there are no conflicts of interest.










