In 2014, one of us (Jacobs Reference Jacobs2014) wrote an article for BJPsych Advances which explained a new method of funding that was being rolled out in England's National Health Service (NHS) for mental health service providers. This approach, then termed payment by results (PbR), was to represent a fundamental change to the way providers of psychiatric services are paid for the care of patients.
Now, 4 years on, it is opportune to take stock of how things have developed, provide an update on how the sector has responded to the proposed funding approaches and reflect on what the funding landscape means for clinicians and services.
A key development since 2014 has been the proposal of not one, but two new payment approaches to replace block contracts for mental health services in England (NHS Improvement 2016). The first approach, formerly termed PbR and now referred to as the National Tariff Payment System (NTPS), is an episodic payment model. Under this approach, a provider is paid a fixed price or tariff for the care provided to a patient during an agreed time frame or episode. The tariff is specific to the mental health needs of the patient and a mental health clustering tool (MHCT) was developed to categorise these relative needs (Self Reference Self, Rigby and Leggett2008). Twenty clusters have been developed as part of the classification system and the cost of treating patients in different clusters is recorded by service providers. The data collected are used to calculate national or local average costs for patient care in each cluster. The ultimate goal of this funding approach is the creation of a fixed price for each care cluster that could then be used to pay services and may help to support cost control.
The second proposed payment approach, termed the capitated payment model, is where a provider is paid to cover a range of care for a whole population. The provider is paid on the basis of the number of people in the relevant population and the payments are risk-adjusted to reflect the complexity and needs of people with mental illness in that population. Mental health activity data are crucial to identifying the mental health population that may need care (NHS England 2016a), and adjusting payment for the population's needs and the proportion of patients within each cluster could serve as one of the mechanisms for risk adjustment, although other approaches are possible, along with other factors, such as age and gender proportions within the population.
But what are the advantages and disadvantages of the two payment approaches? How do quality and outcomes indicators fit into either of the payment systems? Have mental health services introduced either approach? And where does this leave the collection of care cluster data by clinical teams?
In summary, there is a classification or clustering system that was originally developed with a view to using it as a basis for payment, and there is a new suggested approach to payment being developed that seems to not require clustering at all. In the rest of this article we attempt to unravel this paradox and answer two fundamental questions. Does the present clustering system fulfil its purpose? Does clustering still matter? We start by providing some more details of the two payment systems, how they are supposed to work, how they link to quality and outcomes and what they require to operate. We then set out the role that clustering can play and summarise what we have found regarding whether the current clustering system is fit for purpose.
Two payment approaches for mental health services
At present, NHS mental health services in England are primarily funded through block contracts agreed between commissioners and providers of care. A block contract is a payment made to a provider to deliver a broadly defined service: for example, a hospital could be given a block contract to provide mental health services in a particular geographical area. Under block contracts an agreed fixed sum is paid regardless of the number of patients treated. Among the perceived problems with this method of financing is that it encourages hospitals neither to control costs nor to increase output (activity levels) (Mason Reference Mason, Goddard and Myers2011).
Although there are certain advantages to block contracts (they require little in the way of data and monitoring costs are low, they are easy to contract for and provide stable funding since they are usually based on historical funding patterns), there are clear disadvantages (they are not transparent and it is unclear what value for money is being obtained for a given level of expenditure). The two new payment approaches seek to overcome these disadvantages.
Episodic payment approach
The predominant mode of paying for acute physical healthcare in England remains the episodic payment approach, in which healthcare resource groups (HRGs) – standard groupings of clinically similar treatments that use common levels of healthcare resource – represent units of activity or episodes of care, for which a fixed price or national tariff is set. There are over 1400 mandatory tariffs, representing around 60% of payments made to hospitals in England (British Medical Association 2017a) and this approach is the dominant form of payment in most high-income countries.
Previous articles in this journal (Fairbairn Reference Fairbairn2007; Oyebode Reference Oyebode2007; Bhaumik Reference Bhaumik, Devapriam and Gangadharan2011; Jacobs Reference Jacobs2014; Yeomans Reference Yeomans2014) have highlighted the potential advantages and disadvantages of introducing this form of payment system to mental healthcare, and these are outlined in Box 1.
BOX 1 Advantages and disadvantages of an episodic payment approach
Advantages
• Incentive to control unit costs and improve efficiency
• Incentive to increase activity levels and potentially reduce waiting times
• Transparent funding approach for commissioners
• Can support patient choice
Disadvantages
• Providers may ‘cherry pick’ low-risk patients and ‘dump’ high-risk patients (Ellis Reference Ellis1998)
• Under-provision in order to minimise costs (e.g. skimping on quality and intensity of treatment) (Ellis Reference Ellis1998)
• Upcoding of severity of patients’ illness to categories with higher remuneration
• Requires good-quality data and coding
• Does not incentivise integration of care or services
The dominance of this funding approach in physical healthcare is, however, diminishing as it is increasingly being seen as unsustainable. NHS England and NHS Improvement now seek to find new ways to pay providers to support implementation of new models of care proposed in the Five Year Forward View (Mental Health Taskforce 2016; Naylor Reference Naylor, Taggart and Charles2017).
One of the key reasons for the shift away from the tariff payment approach for acute physical care is that the focus on specific procedures can lead to fragmented care and does not facilitate a coordinated approach to healthcare delivery across sectors. This can discourage the treatment of patients in out-of-hospital settings. It is therefore seen as a major barrier to the development of integrated care (British Medical Association 2017a), which is a key plank of current policy.
Sustainability and transformation partnerships (STPs) are now the main mechanism for delivering the Forward View and are seen as a vehicle for developing more integrated approaches between mental and physical healthcare. In STPs, NHS organisations and local authorities in different parts of England come together to develop 5-year ‘place-based’ plans for health and social care services in their area. There are 44 STP areas, each covering an average population of 1.2 million people (King's Fund 2017).
Some of the more advanced STPs are now evolving to become accountable care systems (ACSs) and these have more recently been rebranded as integrated care systems (ICSs) (NHS England 2018). These systems have no statutory basis, but are areas in which commissioners and providers, in partnership with local authorities, are willing to work together to take explicit collective responsibility for resources and population health. These systems effectively dissolve the boundaries between commissioners and providers. ICSs should in principle have greater freedom and control over the operation of their local health system and how funding is deployed. There are currently ten ICSs that are working out the financial, contracting and risk-sharing arrangements to make these systems sustainable (King's Fund 2018).
A proposed further development is accountable care organisations (ACOs), which are a more formal version of an ICS that supposedly simplifies contracting by bringing together funding streams and allowing commissioners to hold a single contract with a single provider, who takes responsibility for deciding how to allocate resources and design care for the local population (British Medical Association 2017b). This can include primary care, hospital care and community care. Providers within an ACO can share any ‘savings’ to the public budget that are achieved (Pollock Reference Pollock and Roderick2018). Most parts of the country may become ICSs before considering whether to introduce ACOs, which as yet do not exist and are the subject of legal challenges (Dyer Reference Dyer2018). These challenges are on the basis that ACO decisions will be taken by non-statutory bodies that may lack public accountability. They will subsume some of the functions of clinical commissioning groups (CCGs) and legislation will be needed for ACOs to replace CCGs. All STPs should become ACSs over the next few years, but it will take considerably longer before ACSs formally become ACOs (Moberly Reference Moberly2017), if at all.
It was the reduced incentive to integrate care under the episodic payment approach, together with the increased ability to foster integration under these new organisational arrangements, that led to the development of STPs (and ICSs and ultimately ACOs) and acted as a major driver towards the capitation payment approach, which is seen as a means of contracting and paying for care within these new geographic footprints.
Capitated payment approach
Capitation is a payment system whereby a lump-sum payment based on the number of patients in a target population is made to a provider or group of providers, to provide some or all of their care needs (British Medical Association 2017a). Like a block contract, the capitation payment is not linked to how many patients are treated. Capitation is often seen as a means to integrate services, particularly mental and physical healthcare, where the provider is responsible for all the health needs of mental health patients. For example, withinan STP local footprint, acute and mental healthcare providers will be jointly responsible for the physical and mental health of their population. In essence, capitation is a means of pricing a form of ‘block contract’, in that the population needs or risks have to be defined so that a per person price can be defined.
The potential advantages and disadvantages of a capitation approach are very similar to those of a block contract and are outlined in Box 2 (Monitor 2015).
BOX 2 Advantages and disadvantages of a capitation payment approach
Advantages
• Incentive to invest in early intervention and prevention to reduce ‘downstream’ costs
• More flexible allocation of resources to improve efficiency
• Incentive to coordinate and integrate health and social care services
Disadvantages
• Providers may ‘cherry pick’ low-risk patients and ‘dump’ high-risk patients (Ellis Reference Ellis1998)
• Under-provision in order to minimise costs (e.g. skimping on quality and intensity of treatment) (Ellis Reference Ellis1998)
• Requires good data to track activity, costs and outcomes for individual patients across different sectors
• Risk of cost shifting if service and population scope are not clearly defined
• Requires significant capabilities on the provider side to coordinate different providers and sectors (e.g. primary, secondary and social care)
Capitation may encourage greater investment in preventive care and care delivered in community settings, because it should give providers greater flexibility to spend money in the areas of a care pathway where they believe it will deliver the best outcomes for patients (British Medical Association 2017a). However, there needs to be a clear mechanism to take account of quality and risk as part of capitated budgets. Arrangements for sharing of risk and financial gain/loss can be difficult to agree and operationalise in practice. The approach therefore demands high-quality data to (a) measure quality and outcomes, both of which are notoriously difficult to agree and measure; and (b) develop risk-adjustment mechanisms on demand levels to ensure that the system can cope financially.
Most STPs being developed and operationalised in England aspire to move towards an outcome-based capitated approach for their populations, which would mean that clinicians would need to document their outcomes, while payment would be delivered on a per person basis to their provider according to the overall needs of their population and not the individual patient, but adjusted for aggregate outcomes. How this payment approach is to be implemented for mental healthcare within these complex geographic footprints and care networks is as yet unclear. Ultimately, under an ACO, the intention is that population-based capitation payments will be derived from current CCG expenditure, although there will be significant challenges in deriving risk-adjusted capitation and risk-pooling (Pollock Reference Pollock and Roderick2018).
Linking quality and outcomes to payment
Under either of these payment approaches, linking quality and outcome indicators to payment is a high priority. This is because under either approach, there is a real risk that providers will skimp on quality. Either payment system therefore needs to be linked to metrics of care quality and outcomes for individual patients (NHS England 2016b). Guidance suggests that a combination of both national and local measures should be used, ones that include both physical and mental healthcare, and that reflect both clinical and social outcomes (NHS England 2016b). Other potential criteria include the need for waiting-time standards to be included and for the co-production of indicators with patients.
An example framework of potential quality and outcome indicators as proposed by NHS England is shown in Table 1. These cover a range of quality and process as well as outcome measures. Some are being routinely collected in services, whereas others may be more challenging to collect. Guidance suggests that a set of three to seven outcome measures with between six and fifteen indicators should be used to link to payment at the contract level (NHS England 2016c).
TABLE 1 Examples of outcome and process measures in mental healthcare that NHS England suggests can be linked to payment approaches

Source: after NHS England & NHS Improvement (2016b: p. 12).
Our research (Moran Reference Moran and Jacobs2015, Reference Moran, Jacobs and Mason2017) shows that the type of quality or outcome metric may matter in the design of the payment system and its selection should be based on sound evidence. The collection and use of these performance indicators within a payment framework may also have unintended consequences`. Any approach will clearly require high-quality and timely data to operate effectively.
There are currently a few examples in the mental healthcare sector of where payment is attached to outcomes, but not many where outcomes are linked to clusters for payment purposes. Policy makers are now considering ways to link specific clusters, for example for psychosis, to evidence-based care and set a best-practice tariff that is linked to outcomes. One challenge is that much National Institute for Health and Care Excellence (NICE) guidance for mental health pre-dates the use of care clusters and therefore does not simply map onto them in terms of recommendations of best practice.
Which approach to use? And what is happening in reality?
Evidence suggests that, despite guidance (Monitor 2016) to the sector that it move away from block contracts, very few providers/commissioners have indeed done so. A handful of providers have adopted the episodic payment approach, but capitation approaches are currently seen as difficult to adopt since the data are not yet adequate to risk adjust appropriately. Our research has shown that the choice of payment options has in fact caused much confusion among commissioners (Jacobs Reference Jacobs, Chalkley and Aragòn2016) and they have felt uncertain as to which approach to adopt and how to do it. Some felt they ought to be developing capitation models to be keeping up with the latest thinking. However, this felt like a big step from their current practice of using block contracts, because they were not able to meet data requirements that would give them adequate understanding of population risk in their region and/or because it seemed that they would be abandoning their work on episodic models, which have a stronger evidence base, before they had a chance to learn fully about this new approach to commissioning.
Extrapolating from our understanding of the evidence base about forms of payments and issues of data quality, the notion of a capitation model as a way forward seems to pose significant challenges. There is, however, little in the way of robust evidence about the performance of capitation models in the context of mental healthcare in England, chiefly because they are new, although there are some international examples (Monitor 2014). Indeed, there is little evidence comparing a capitation with an episodic payment system. This makes it difficult to determine the best model in terms of its overall cost-effectiveness and its utility as a means of managing fragmentation/integration risks.
We would argue that the episodic payment approach has a number of advantages over the capitated payment approach, including stronger incentives to increase activity rates and control costs. It may also be simpler to implement from a contracting perspective and, given capacity constraints among commissioners, may be more pragmatic since it may be less prone to problems in terms of the quality of partnerships or which organisations within a local health economy are running a deficit. Episodic payment is a more transparent funding approach than capitated payment. The episodic payment approach therefore has the potential to establish greater parity of esteem between mental and physical healthcare, although it is the case that acute physical health services are slowly moving away from episodic payment and this argument may not hold in the future.
Two aspects are, however, common between the two approaches and both are fundamental to the operation of any payment model:
• the need for high-quality, timely data as part of a classification system that defines a measure of activity – for example, a diagnosis or a cluster
• the need for valid and reliable measures of quality and outcomes that can be linked to the classification system.
Although the use of diagnoses could be a valuable addition to a classification system, most countries have found that diagnoses alone are not sufficient to identify need within a mental health payment framework (Mason Reference Mason, Goddard and Myers2011).
Why do we need clustering?
The episodic and capitated payment approaches rely on a classification system that effectively categorises patients' symptoms and needs. However, unless mental health activity is recorded and classified in a way that provides strong evidence of what funding achieves, it is at continuing risk of being funded inadequately. Why? Because in any system in which the financial resources follow patients and their needs, it is ultimately healthcare activity that is used as the metric of need – and hence determines funding. Mental health clusters therefore continue to be an important tool both locally and nationally (NHS Improvement 2016):
• in local pricing arrangements as a source of activity data, and
• in both capitated and episodic payment approaches.
Our research (Jacobs Reference Jacobs, Chalkley and Aragòn2016) showed that commissioners welcome the care cluster model and use it as a framework to understand and discuss local patterns of care and variations.
In both payment systems, clusters should be essential to either (a) assign patients to resource-homogeneous groups, or (b) define a unit of activity for resource allocation. Clusters can help identify the level of resources needed to treat different groups of patients and therefore allow the provider to ‘claim’ resources according to the activity it performs. Care clusters provide the basis for a classification system that makes mental health services more transparent and accountable.
How is clustering working?
The key challenge for any payment approach is to introduce a classification system that accurately and consistently captures similarities and differences between patients. The categories of such a classification system need to be homogeneous in terms of both case-mix and resources, that is, patients within a given care cluster have similar needs profiles and their treatment requires approximately similar levels of resources. Our research (Jacobs Reference Jacobs, Chalkley and Aragòn2016) shows that there is enormous variation within the current clusters in terms of activity and costs. Considerable variation in levels of need and case-mix within care clusters was anticipated from the outset (Bhaumik Reference Bhaumik, Devapriam and Gangadharan2011; Jacobs Reference Jacobs2014). However, the problem with high levels of variation within clusters is that accurate baseline activity cannot be determined for commissioning purposes. And high levels of cost variation within clusters make it difficult to set prices or tariffs.
We are concerned about not only absolute levels of activity and costs, but also the relative variation between providers in costs and activity rates. Our research shows that the variation in activity rates between providers is substantial. Variation in activity rates means that providers see different numbers of patients, have different levels of productivity, and put different care pathways and packages of care in place for patients with similar levels of need. This suggests differences in the quality of care that patients receive across providers, generating potential geographic inequalities for patients. Variations in costs mean that patients with similar levels of need as defined by the MHCT may be receiving different levels of resource, or again that there is inequality between patients in what care they receive because of where they live. The reduction of variation in care, activity levels and costs is therefore pivotal to the establishment of a well-designed classification and payment system.
To examine these sources of variation, we did an evaluation of whether the data collected in the Mental Health Minimum Dataset (MHMDS) (now called the Mental Health Services Dataset, MHSDS) can provide accurate measures of activity among mental health providers, and it showed significant variability also in activity and resource use within clusters (Jacobs Reference Jacobs, Chalkley and Aragòn2016). The measure of activity was the number of cluster days (the number of days assigned to a cluster episode), while the measure of resource use was (a) the number of admitted (in-patient) days and (b) the number of days with contact with a healthcare professional. We used MHMDS data for the periods 2012–2013 and 2013–2014.
One of the issues identified (Jacobs Reference Jacobs, Chalkley and Aragòn2016) was the differences in the length of the cluster episodes among providers. If all providers were delivering the same care but were reporting it at different intervals we would observe something like Fig. 1, where longer cluster episodes have the same proportion of resource use, in terms of both admitted days and days with contact with a healthcare professional, as shorter episodes.
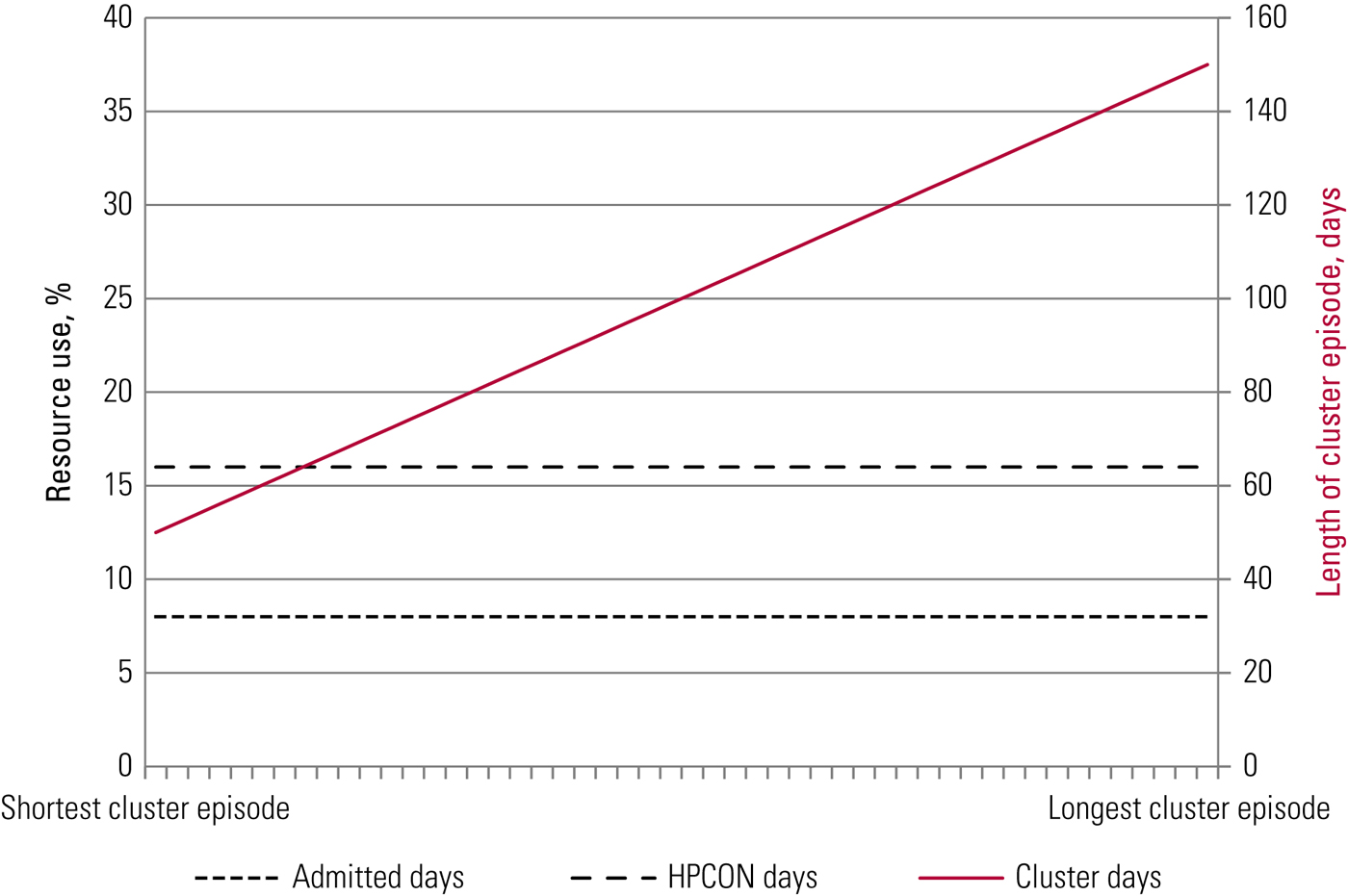
FIG 1 A hypothetical activity cluster. The x-axis represents each of the approximately 50 mental healthcare providers in the NHS, ordered by increasing size of their reported number of cluster days for this particular hypothetical cluster. The measure of resource use is (a) the number of admitted (in-patient) days and (b) the number of days with contact with a healthcare professional (HPCON days).
Figure 2 shows the actual length of cluster episodes and activity and resource use for cluster 10 (first episode of psychosis) as an example, using MHMDS data. We see that longer cluster episodes do not translate into proportionally more activity (admitted days) and resource use (days with contact with a healthcare professional), as anticipated. The sources of this variation are not clear, some of it is the result of data-quality problems, but this variation also points to actual differences between providers, in terms of practice and/or allocation to clusters.
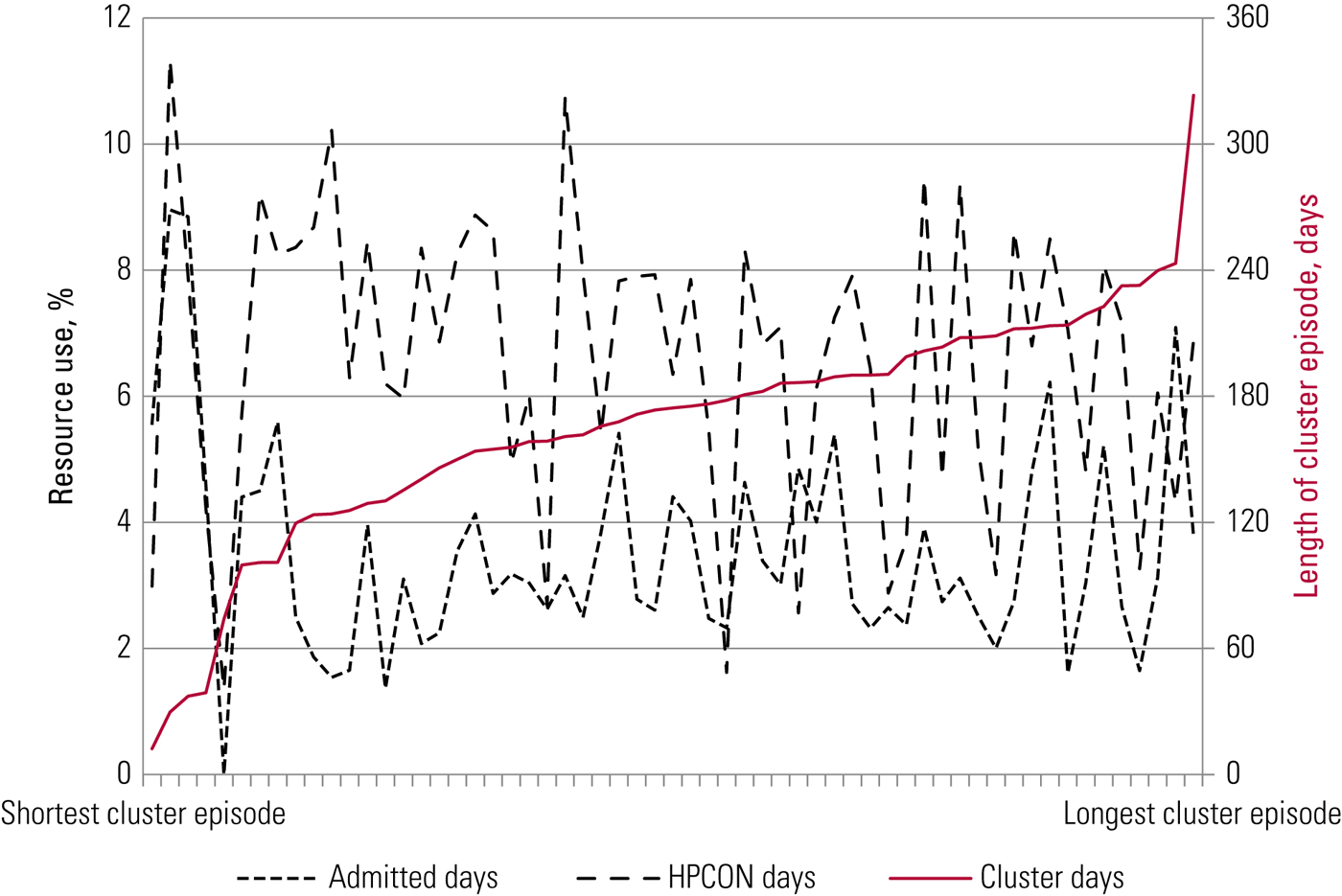
FIG 2 Activity in an actual cluster. The x-axis represents each of the approximately 50 mental healthcare providers in the NHS, ordered by increasing size of their reported number of cluster days for cluster 10 (first episode of psychosis). The measure of resource use is (a) the number of admitted (in-patient) days and (b) the number of days with contact with a healthcare professional (HPCON days).
We found very similar patterns of variation within clusters and between providers for all 20 care clusters (Jacobs Reference Jacobs, Chalkley and Aragòn2016), i.e. there is substantial variability across providers in the length of cluster episodes (activity) and there is substantial variability within clusters in terms of the proportion of admitted days and the proportion of contact with healthcare professionals (resource use).
Authors have also drawn attention to the limitations with respect to the costing of clusters, in particular a lack of homogeneity in costs for care clusters (Bhaumik Reference Bhaumik, Devapriam and Gangadharan2011; Jacobs Reference Jacobs2014). Our research (Jacobs Reference Jacobs, Chalkley and Aragòn2016) also provides evidence of significant variation in cluster costs between providers: costs reported by the most expensive provider are 55% higher than average, whereas those of the least expensive provider are 25% below average. The ratio between the provider with the highest costs and the one with lowest is around 2:1, but in some clusters this ratio can be as high as 10:1. Looking within clusters, those with large variability in costs include clusters 1 (Common mental health problems (low severity)), 2 (Common mental health problems), 15 (Severe psychotic depression), 18 (Cognitive impairment (low need)), 19 (Cognitive impairment or dementia (moderate need)) and 21 (Cognitive impairment or dementia (high physical need or engagement)).
Do we abandon clustering? No!
Clusters are therefore not performing very well as a classification system to capture similarities and differences between patients. The categories of the current classification system appear to be neither case-mix nor resource homogeneous. We find evidence of large variation in terms of activity and costs within clusters and between providers.
This would seem to suggest that it would be best to dismantle the clustering approach altogether. Indeed, there have been calls from many corners expressing such views (Royal College of Psychiatrists 2014). However, we would argue that any payment approach needs to be underpinned by a solid classification system and to abandon the clustering approach now will thwart all progress. The clustering approach is already relatively well-established among most providers. Scrapping it all and starting from scratch risks putting mental health services back a decade in terms of developing a more transparent and fair funding system.
The key reason not to abandon clustering is that, in the absence of such a classification system, mental health would be deprived of resources. Most CCGs have contracts with acute physical healthcare providers in which they must pay according to the activity performed, whereas providers of care in other settings, such as community and mental healthcare, are usually paid on the basis of block contracts. If acute activity levels increase, CCGs must try to pay for that increased activity, leaving, if their budgets do not grow accordingly, fewer resources to allocate among the other care settings. However, actual behaviour may diverge from the contractual position if CCG budgets are insufficient (Allen Reference Allen and Petsoulas2016).
The argument of the ‘institutional bias’ towards acute providers in the funding system is well rehearsed, often seeing larger cuts for mental health services compared with acute services (King's Fund 2015). Given the current and future projected financial position of providers, with mental health providers generally delivering overall surpluses year on year, compared with huge increases in deficits in recent years for acute providers (Dunn Reference Dunn, McKenna and Murray2016), mental health services have been at risk of having their resources diverted to acute providers. The lack of a transparent funding system for mental healthcare is a major risk factor. As long as there are parallel funding systems operating, where in one, better-quality activity data and a more transparent classification system (episodic payment) make the return on investment of limited budgets more obvious, that payment approach will always win out. Thus, as long as mental healthcare operates a block contract system and does not use a transparent classification system, commissioners will not have a clear sense of the value for money they are getting from investment in these services. Even if both acute and mental healthcare providers move towards a capitation approach under an STP, the argument for a strong and transparent classification system remains.
Although the current cluster system does not work as well as it should, rather than abandon the system we need to make it work better, to ensure fair and consistent funding (Oyebode Reference Oyebode2007) and to prevent an unfair reduction in investment in mental health services (Fairbairn Reference Fairbairn2007; Bhaumik Reference Bhaumik, Devapriam and Gangadharan2011; Jacobs Reference Jacobs2014).
What should be done?
• A continued commitment from clinical teams to cluster mental health patients is required. Since clustering is built on an outcome measure, the Health of the Nation Outcome Scales (HoNOS), providers need to find mechanisms to feed back outcomes to clinical staff in a meaningful way that will reduce concerns over clustering being seen as a paper-filling exercise for managers (Jacobs Reference Jacobs and Moran2010).
• Clusters need to be linked to care pathways and evidence-based care (as recommended in NICE guidelines), so that they can be linked to measures of quality and contribute to better patient outcomes.
• The MHCT should be refined in order to establish more homogeneous groupings of patients.
• The classification system requires a wider range of complexity (more clusters), just as HRGs have increased in number and the clinical labels have become more specific.
• Most important of all, there needs to be a significant improvement in data quality, for both costs and activity. A programme to implement the new payment models needs to be supported to ensure that all clinicians and services collect reliable data about classifications, care quality and outcomes. Significant investment in information technology is required and improvement in data quality needs to be a priority in mental health services. The MHSDS is not yet suitable for use as an information tool to accurately count activity, which would be central to its use as a platform for the payment system. To develop it for this use, all commissioners and providers should routinely use only the MHSDS in their contracting and monitoring processes. This will facilitate a single consistent use of data across all commissioners with any given provider and prevent providers wasting resources filling in different dataset requirements for different commissioners. It will also incentivise rapid improvement in the data quality of the MHSDS because it can be used by all commissioners and providers to benchmark activity.
So, although clustering patients may seem a tedious or pointless requirement for clinical teams, it is crucial for the overall financial sustainability of the mental health sector. NHS England has already recognised the need to strengthen the clinical relevance of clusters in relation to clinical care pathways (NHS Improvement 2016).
Conclusions
There is continuing debate about how best to organise a funding model for mental healthcare, as with other healthcare. Mental healthcare lagged behind physical healthcare in not implementing an episodic payment system. It is now caught between systems (block grants – an emerging but underdeveloped episodic system – and an ill-defined, aspirational capitation system). The risk in all this of confusion is that commissioners and providers will fail to develop a robust payment system that links fair payments to high-quality care and good outcomes for patients. A payment system is needed that could be used to support service improvements and better patient outcomes. Whatever system is adopted, some form of classification of patients related to their conditions and needs will be imperative. If we scrap the current system of care clusters we will have to go back to square one and it is not very clear how else we would move on from there, nor how long that would take. The care clusters are flawed in the ways that we have demonstrated above, but knowing their flaws and having a reasonable empirical basis to understand their use provides us with an opportunity to improve the clinical and financial bases of the clusters and to move forward with putting mental healthcare onto a firmer and fairer approach to its funding.
Data quality is a significant challenge with any payment system, but data collection is at least underway using clustering, and collected routinely. Our key recommendations related to cluster are as follows.
• clinical teams must continue to collect clustering data and they should be given meaningful routine feedback of HoNOS ratings, which underpin the MHCT, so that the collected data can be effectively utilised
• clusters need to be linked to care pathways and the evidence-based care in NICE guidelines so that they can be linked to measures of quality and contribute to better outcomes for patients
• the MHCT should be refined to establish more homogeneous groupings of patients
• the classification system requires a wider range of complexity (more clusters)
• and there needs to be a significant improvement in data quality, for both costs and activity: this requires providers to invest in information technology and commissioners to commit to using only the MHSDS in their contracting processes.
Acknowledgements
This work was part-funded by the Wellcome Trust (ref: 105624) through the Centre for Chronic Diseases and Disorders (C2D2) at the University of York. The views expressed in this article are the authors' and not the funder's, and any errors or omissions that remain are our responsibility.
MCQs
Select the single best option for each question stem
1 Both capitation and episodic payment approaches potentially create incentives for:
a under-provision of services
b over-provision of services
c duplication of services
d providing more expensive services
e longer length of stay.
2 Block contracts are characterised by:
a a fixed-sum payment
b a payment that does not take account of the number of patients treated
c relatively easy contracting arrangements
d a lack of transparency
e all of the above.
3 A capitated payment system:
a may discourage preventive care
b provides good data to track patient care activity
c requires a risk-adjusted price per person to be defined
d is linked to the number of patients treated
e disincentivises integrated care.
4 Clusters:
a are a diagnostic classification
b are a good discriminator of cost variation
c are used to underpin block contracts
d show large variation in activity between providers
e can be used as an outcome.
5 Clustering is needed:
a to categorise patients with similar levels of need
b to define levels of activity
c to understand local patterns of care and variation
d to underpin a more transparent funding system
e all of the above.
MCQ answers
1 a 2 e 3 c 4 d 5 e






eLetters
No eLetters have been published for this article.