No CrossRef data available.
Article contents
Impact of exposure to potentially contaminated hospital beds on risk of hospital-onset C. difficile infection
Published online by Cambridge University Press: 16 May 2022
Abstract
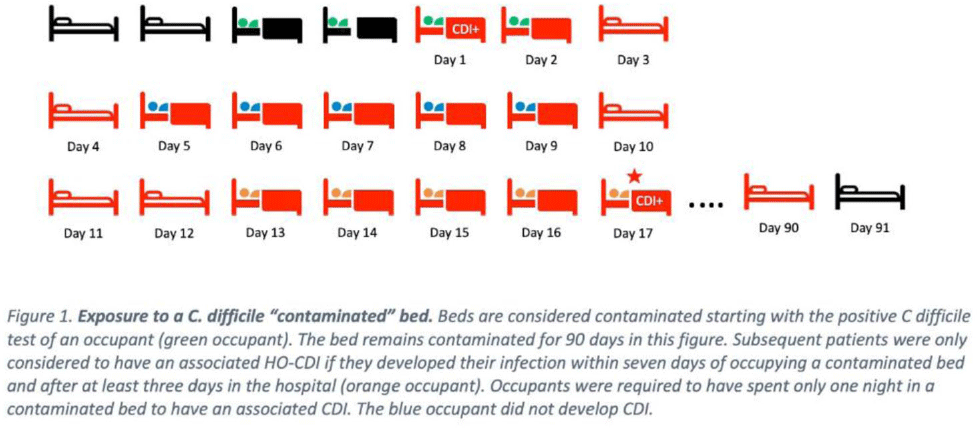
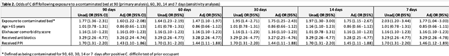
Background: Environmental contamination increases risk for Clostridioides difficile infection (CDI) given that spores can remain on a hospital bed, floor, sink, and light switch despite appropriate cleaning measures. Using real-time asset management software (AgileTrac, GE Healthcare) for beds we examined the risk of a patient developing hospital-onset CDI (HO-CDI) when staying in a hospital bed that had a previous occupant with CDI. Methods: We retrospectively identified all patients in tracked beds from April 2018 to August 2019 to identify hospital-onset CDI (HO-CDI), defined as a positive PCR test for C. difficile in a patient hospitalized for >3 days. A patient was defined as being exposed to a potentially “contaminated” bed if within the preceding 7 days from their HO-CDI diagnosis they resided in a hospital bed that, within the prior 90 days, had held an occupant with CDI (Fig. 1). We used multivariable logistic regression to evaluate the association between being exposed to a contaminated bed and HO-CDI. Model covariates were chosen a priori based on known risk factors for CDI. As a sensitivity analysis, we varied the length of time that a bed could stay contaminated from 90 to 60, 30, 14, and 7 days. Results: We analyzed 25,032 hospital encounters representing 18,860 unique patients; we identified 237 (0.9%) hospital encounters with HO-CDI (Table 1). The Elixhauser comorbidity score, being exposed to a contaminated bed, and receiving antibiotics or a proton pump inhibitor (PPI) during the hospital admission were all associated with HO-CDI in the univariable analysis (Table 2). In the adjusted multivariable model, being exposed to a contaminated bed remained a significant risk factor for HO-CDI (OR, 1.60; 95% CI, 1.22–2.08) even after controlling for known risk factors for CDI including age >65, elevated Elixhauser score, and recent antibiotic or PPI use (Table 2). In the sensitivity analysis in which we adjusted the time a bed was considered contaminated after CDI, being exposed to a contaminated bed remained a risk factor for HO-CDI, with a similar odds ratios as the original model (Table 2). Conclusions: Residing in a hospital bed that contained a previous occupant with CDI is a risk factor for developing HO-CDI. Hospital epidemiologists, infection control personnel, and environmental services staff should consider this association when developing CDI risk mitigation strategies.
Funding: None
Disclosures: None

- Type
- C. difficile
- Information
- Antimicrobial Stewardship & Healthcare Epidemiology , Volume 2 , Issue S1: SHEA Spring 2022 Abstracts , July 2022 , pp. s17 - s18
- Creative Commons
- This is an Open Access article, distributed under the terms of the Creative Commons Attribution licence (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted re-use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Copyright
- © The Author(s), 2022. Published by Cambridge University Press on behalf of The Society for Healthcare Epidemiology of America


