Introduction
In an era of patient-centred care, long-term care (LTC) settings have been heavily critiqued (Koren, Reference Koren2010), with some going so far as to call for the dismantling of these care settings in response to observed inadequacies. Yet, LTC is an increasingly universal response to human need (Katz, Reference Katz2011). Although LTC settings serve a very diverse population, more and more, they are serving those who are dying of dementia, frailty and other chronic health conditions (Hirdes et al., Reference Hirdes, Mitchell, Maxwell and White2011; Doupe et al., Reference Doupe, John, Chateau, Strang, Smele, Bozat-Emre, Fransoo and Dik2012). This leaves the question, for those who need it, how can LTC settings create the organisational conditions that best achieve a humane, person-centred approach to care for residents in their last months or years of life?
Research has identified that many LTC employees seek meaningful work in a highly relational context (Kemp et al., Reference Kemp, Ball, Perkins, Hollingsworth and Lepore2009). They frequently intend to provide person-centred care, or a humanistic approach that prioritises quality of life as uniquely defined by an individual over institutional or health-related goals (Li and Porock, Reference Li and Porock2014), scoring high on measures of self-reported humanism, and articulating person-centred values that provide meaning in work (Hunter et al., Reference Hunter, Hadjistavropoulos, Smythe, Malloy, Kaasalainen and Williams2013, Reference Hunter, Hadjistavropoulos and Kaasalainen2016a; Vidman and Strömberg, Reference Vidman and Strömberg2018; Vassbø et al., Reference Vassbø, Kirkevold, Edvardsson, Sjögren, Lood and Bergland2019). Yet, despite the best intentions and efforts of most health-care providers, many reports suggest that LTC continues to fall short of the mark (Estabrooks et al., Reference Estabrooks, Straus, Flood, Keefe, Armstrong, Donner and Wolfson2020). Studies of person-centred care have identified several potentially relevant explanatory factors, extending from individual health-care provider characteristics to organisation and system-level factors.
At the level of the individual, certain demographic factors have been associated with person-centred attitudes. For example, increasing health-care provider age is associated with less person-centred attitudes in some studies (Kada et al., Reference Kada, Nygaard, Mukesh and Geitung2009; Nilsson et al., Reference Nilsson, Lindkvist, Rasmussen and Edvardsson2012; Scerri et al., Reference Scerri, Innes and Scerri2020), although not universally (Åström et al., Reference Åström, Nilsson, Norberg, Sandman and Winblad1991; Brodaty et al., Reference Brodaty, Draper and Low2003; Sjögren et al., Reference Sjögren, Lindkvist, Sandman, Zingmark and Edvardsson2015). Studies of the relationship between years of work experience and person-centredness also offer mixed results (Åström et al., Reference Åström, Nilsson, Norberg, Sandman and Winblad1991; Brodaty et al., Reference Brodaty, Draper and Low2003; Zimmerman et al., Reference Zimmerman, Williams, Reed, Boustani, Preisser, Heck and Sloane2005; Kada et al., Reference Kada, Nygaard, Mukesh and Geitung2009). A small relationship between gender and person-centred care is identified in some studies, with women showing more positive attitudes towards patients (Sjögren et al., Reference Sjögren, Lindkvist, Sandman, Zingmark and Edvardsson2015; Scerri et al., Reference Scerri, Innes and Scerri2020), but other studies have failed to demonstrate such a relationship (Åström et al., Reference Åström, Nilsson, Norberg, Sandman and Winblad1991; Brodaty et al., Reference Brodaty, Draper and Low2003; Kada et al., Reference Kada, Nygaard, Mukesh and Geitung2009) or have found that specialised training reduces effects of gender (Keogh et al., Reference Keogh, To, Daly, Hynes, Kennelly, Lawlor, Timmons, O'Reilly, Bracken-Scally, Ciblis, Cole, Drury, Pittalis, Kennelly, McCarron and Brady2020). Overall, these results suggest that studying the relationship between demographic variables and person-centredness may be important. This approach is also limited since these factors cannot be modified.
Modifiable personal characteristics, including education level, employee wellbeing and self-efficacy, have also been studied in relation to person-centred care. Education level is associated with person-centred attitudes and responses (Macdonald and Woods, Reference Macdonald and Woods2005; Kada et al., Reference Kada, Nygaard, Mukesh and Geitung2009; Hunter et al., Reference Hunter, Hadjistavropoulos, Thorpe, Lix and Malloy2016b; Foster et al., Reference Foster, Balmer, Gott, Frey, Robinson and Boyd2019). There is also evidence that having knowledge of the population one's work serves is positively correlated with person-centred care (Sjögren et al., Reference Sjögren, Lindkvist, Sandman, Zingmark and Edvardsson2015), and that education specifically focused on person-centred care components results in better person-centred dementia care (Rokstad et al., Reference Rokstad, Døble, Engedal, Kirkevold, Benth and Selbæk2017). Burnout, too, is associated with reduced person-centredness (Hunter et al., Reference Hunter, Hadjistavropoulos, Thorpe, Lix and Malloy2016b), as implied in the construct itself, which includes attention to ‘depersonalisation’ (Maslach and Jackson, Reference Maslach, Jackson and Leiter1996). Finally, self-efficacy, which measures employees' perceptions of their own capabilities for specific work skills, is important to health-care quality (Bandura, Reference Bandura1986) and a range of work performance outcomes (Stajkovic and Luthans, Reference Stajkovic and Luthans1998).
Alongside these promising developments in understanding how individual variables might shape the provision of humanistic care, there is also evidence to suggest that the contexts within which employees work greatly influence person-centred care. While care assistants describe person-centred goals for their work, they also perceive that organisational factors (especially, a pressure for efficiency) compromise their capacity to provide person-centred care (Hunter et al., Reference Hunter, Hadjistavropoulos and Kaasalainen2016a). There is evidence that, relative to for-profit LTC facilities, public-owned and not-for-profit facilities provide superior care to residents (Hsu et al., Reference Hsu, Berta, Coyte and Laporte2016; Ronald et al., Reference Ronald, McGregor, Harrington, Pollock and Lexchin2016; Poss et al., Reference Poss, McGrail, McGregor and Ronald2020), presumably because for-profit homes rely on a leaner staff complement. For example, for-profit homes demonstrated higher hospitalisation rates compared with both public-owned facilities and not-for-profit homes in different Canadian jurisdictions that serve the same population (McGregor et al., Reference McGregor, Tate, McGrail, Ronald, Broemeling and Cohen2006; Tanuseputro et al., Reference Tanuseputro, Chalifoux, Bennett, Gruneir, Bronskill, Walker and Manuel2015).
To achieve a fuller understanding of the relative importance of personal and organisational variables to person-centred care, it is important to examine these variables systematically in relation to each other. In a previous study that relied on statistical modelling to understand the relative importance of employee-level and organisation-level factors to person-centredness, Hunter et al. (Reference Hunter, Hadjistavropoulos, Thorpe, Lix and Malloy2016b) found that organisational factors (i.e. care providers' perceptions of the physical and social environment of the residence, the extent of collaboration on person-centred care, and supervisory or other organisational support) were more important determinants of self-reported person-centred care than employee characteristics, including gender, employee beliefs about personhood and employee wellbeing (e.g. burnout).
The current study focuses on the relative importance of employee and organisational predictors of person-centred palliative care in LTC. Based on previous findings, we hypothesised that among a number of person-level factors (age, gender, education level, professional training, years of work experience, self-efficacy and employee wellbeing), only gender, employee wellbeing and self-efficacy would be associated with person-centred care. In contrast, we hypothesised that all organisational factors (facility size, profit status of the facility and non-hierarchical distribution of work roles) would be associated with three domains of person-centred palliative care, including knowledge of the person, comfort care and supporting relationships. Overall, we expected that person-level factors would be weaker predictors of person-centred care than the organisation-level factors.
Methods
Design
This study used a cross-sectional survey design. The survey included three questionnaires, further described below, and questions about personal demographic characteristics. This study was part of a larger mixed-methods project exploring the implementation of the Strengthening a Palliative Approach in Long Term Care (SPA-LTC; www.spaltc.ca) program in four participating LTC homes using a participatory action approach (Kaasalainen et al., Reference Kaasalainen, Sussman, Thompson, McCleary, Hunter, Venturato, Wickson-Griffiths, Ploeg, Parker, Sinclair, dal Bello-Haas, Earl and You2020). These homes are located in the Canadian provinces of Alberta (<150 residents), Saskatchewan (<75), Manitoba (<125) and Ontario (<300). Three are operated by the same for-profit company, and the fourth is a non-profit entity. In a previous descriptive analysis of data from this survey conducted prior to the implementation of SPA-LTC (Hunter et al., Reference Hunter, McCleary, Akhtar-Danesh, Goodridge, Hadjistavropoulos, Kaasalainen, Sussman, Thompson, Venturato and Wickson-Griffiths2020), we identified strengths and gaps in palliative care readiness among LTC employees. The current analysis focuses on the relative importance of organisation-level and person-level predictors of person-centred palliative care.
Procedure: sampling and data collection
After approval by institutional review boards, we recruited a convenience sample of staff employed at four Canadian LTC facilities. In collaboration with the participating homes, we invited all current employees (e.g. managers and administrators, clerical staff, nurses, social workers, occupational therapists, nursing care assistants, housekeepers, recreation workers, maintenance staff and kitchen staff) to participate in the survey either personally or through workplace mail. A modified Dillman (Reference Dillman1978) approach was used to maximise the response rate. That is, we tracked staff who completed the survey, and followed up with those who did not by extending another invitation. The maximum number of invitations was three. To further encourage participation, we held a draw at each of the participating LTC homes and told staff that they would be entered to win a $50 gift card on completing the survey. Surveys were collected in the manner each LTC context identified as most appropriate to their setting, such as in a locked drop box. Surveys took approximately 30 minutes to complete.
Measures
The survey emphasised three constructs of interest: emotional wellbeing, palliative care self-efficacy and person-centred care. We used the Professional Quality of Life scale (ProQOL; Stamm, Reference Stamm2010) to assess emotional wellbeing, the End-of-Life Professional Caregiver Survey (EOL-PC; Lazenby et al., Reference Lazenby, Ercolano, Schulman-Green and McCorkle2012) to assess palliative care self-efficacy and the Person-Directed Care scale (PDC; White et al., Reference White, Newton-Curtis and Lyons2008) to assess person-centred care. We emphasised aspects of person-centred care that are highly relevant to palliative care, including comfort care, knowing the person and support for relationships. Given our unrestrictive inclusion criteria, we encouraged participants to mark items as inapplicable if necessary, and we did this by modifying the questionnaires to include an ‘inapplicable’ response alongside other possible responses.
Employee wellbeing
The ProQOL version 5 (Stamm, Reference Stamm2010) is a 30-item questionnaire that measures three aspects of employee wellbeing: compassion satisfaction, i.e. feeling fulfilled in one's work; burnout, i.e. feeling overwhelmed by one's work; and secondary traumatic stress, i.e. experiencing problems as a result of work-related exposure to others' trauma. The three ProQOL subscales have good internal consistency reliability, with previously reported Cronbach's alpha coefficient estimates of 0.88, 0.75 and 0.81, respectively (Stamm, Reference Stamm2010), and current estimates of 0.88, 0.74 and 0.81, respectively. Responses are given on a five-point Likert scale. The cut score for both burnout and secondary traumatic stress is 42, meaning that higher scores than this indicate a concern (Stamm, Reference Stamm2010). The cut score for compassion satisfaction is 22; in this case, lower scores indicate a concern.
Palliative care self-efficacy
The EOL-PC (Lazenby et al., Reference Lazenby, Ercolano, Schulman-Green and McCorkle2012) is a 28-item Likert-type scale that measures self-efficacy in three domains of end-of-life care: patient- and family-centred communication (12 items); cultural and ethical values (eight items); and effective care delivery (eight items). A total scale score can be calculated by adding the scores for all 28 items. The scale has shown good internal consistency in other studies (Lazenby et al., Reference Lazenby, Ercolano, Schulman-Green and McCorkle2012). In this study, Cronbach's alpha for the full scale was 0.95.
Person-centred care
The PDC (White et al., Reference White, Newton-Curtis and Lyons2008) is a 35-item questionnaire that measures behaviours associated with person-centred care. Three subscales have high overlap with palliative care domains (Van der Steen et al., Reference Van der Steen, Radbruch, Hertogh, De Boer, Hughes, Larkin, Francke, Jünger, Gove, Firth, Koopmans and Volicer2014): Knowing the Person (seven items), Comfort Care (eight items) and Support for Relationships (six items). Responses are given on a five-point Likert-type scale. For these subscales, previously reported Cronbach's alpha coefficient estimates were 0.91, 0.88 and 0.91, respectively (White et al., Reference White, Newton-Curtis and Lyons2008), and current estimates are 0.90, 0.87 and 0.90, respectively.
Demographics questionnaire
We also used a brief questionnaire to inquire about personal characteristics (including age, gender identity, education level, occupation and years of experience in LTC) and workplace characteristics (including facility, involvement in care planning and involvement in updating resident records).
Analyses
To complete the multiple linear regression analyses described below, we determined that to have 80 per cent power to detect a small effect at the 0.05 significance level using 12 predictors, we would need a sample size of 127. Despite observing occupation-related differences in scores on some measures, none of the occupational groups represented in our sample were sufficiently large to allow this analysis within occupation. We therefore pooled the sample to include all staff involved directly in patient care (i.e. nurses and other regulated professionals, such as social workers; care assistants and other unregulated supporting staff, such as recreation workers), and included occupation as one of the variables in the regression models. To acknowledge more fully some important differences in staff experience, we conducted pooled sample t-tests comparing the responses of the professional and supporting staff groups on each measure. Finally, we calculated the Pearson correlation coefficient for every combination of the variables included in the study.
We then proceeded to conduct a series of three multiple linear regression analyses to examine the association of personal and organisational factors with three aspects of self-reported person-centred care that are relevant to palliative care provision (i.e. comfort care, knowing the person and support for relationships). We used backward stepwise regression to consider not only how the regression models performed as a whole, but also how theoretically relevant groupings (blocks) of variables influenced the performance of each model. Specifically, blocks of variables representing personal characteristics, organisational characteristics, occupational characteristics, palliative care self-efficacy and employee wellbeing were simultaneously regressed on PDC subscale scores. In Block 1 (personal characteristics), we entered the following independent variables: years of work experience, a dummy variable representing education (1 = university degree; 0 = no degree), and a dummy variable representing gender (1 = female; 0 = male and other). In Block 2 (organisational characteristics), we entered the following variables: facility size (1 = small; 0 = medium or large) and facility profit status (1 = non-profit; 2 = for-profit). In Block 3 (job characteristics), we entered a dummy variable representing occupational role (1 = nurse or other professional care staff; 0 = nursing care assistant or other supporting care staff) and another reflecting involvement in care planning (1 = involved; 0 = not involved). Block 4 included two ProQOL subscales assessing employee wellbeing (burnout and compassion satisfaction). Finally, Block 5 included the total score on the EOL-PC, a measure of self-efficacy. The independent contribution of each block of variables was then tested by fitting full and restricted multiple regression models to the data (a full or unrestricted model is one that includes all independent variables, and a restricted model is one in which one or more variables are omitted). To evaluate the independent contribution of each block of variables to the model, we used analysis of variance to test the difference in adjusted R 2 values between the full model and restricted models. A series of comparisons was made by comparing the full model to other models that contained all variables except the block of interest. All significance tests were conducted using α = 0.05.
Results
Sample characteristics
A total of 228 questionnaires were returned, representing a response rate of 32 per cent. After excluding participants who were not involved directly in providing care (i.e. support staff, including housekeepers, food service workers), we obtained a total sample size of 184. Of these, 76 (41%) were professional care staff (most were nurses) and 108 (59%) were supporting care staff, including 105 care assistants and three recreation workers. Of these, 159 (86%) identified as women, 14 (7%) as men and one (0.5%) as non-conforming. An additional ten (5%) did not disclose their gender identity. Age was given as a range, and more than 50 per cent of participants were at least 45 years old. Twenty-eight (15%) of the participants did not have any post-secondary education, while the remainder held degrees (28%) or diplomas (47%).
In Table 1, we report the means and standard deviations for professional and supporting staff on each measure. t-Tests comparing these two occupational groups show that scores on self-efficacy, knowing the person, burnout and secondary trauma differ across occupational groups, while scores on comfort care, support for relationships and compassion satisfaction do not (see Table 1).
Table 1. Sample size, mean, standard deviation (SD) and t-test for self-efficacy, person-directed care and quality of life scores for professional staff and staff in supporting roles

Notes: Max: maximum scale score. ET: established threshold (for compassion satisfaction, scores lower than threshold indicate a concern; for burnout and secondary traumatic stress, scores above the threshold indicate a concern). PDC: Person-Directed Care scale. ProQOL: Professional Quality of Life scale.
Significance level: * p < 0.05.
In Table 2, we report Pearson correlation coefficients for all variables included in the regression models. Statistically significant correlations were observed among several variables, with several showing a moderate effect size (0.3–0.5) and some a large effect size (>0.5) (see Table 2).
Table 2. Inter-correlations among variables assessing employee wellbeing, palliative care self-efficacy, person-centred care, personal characteristics and workplace characteristics
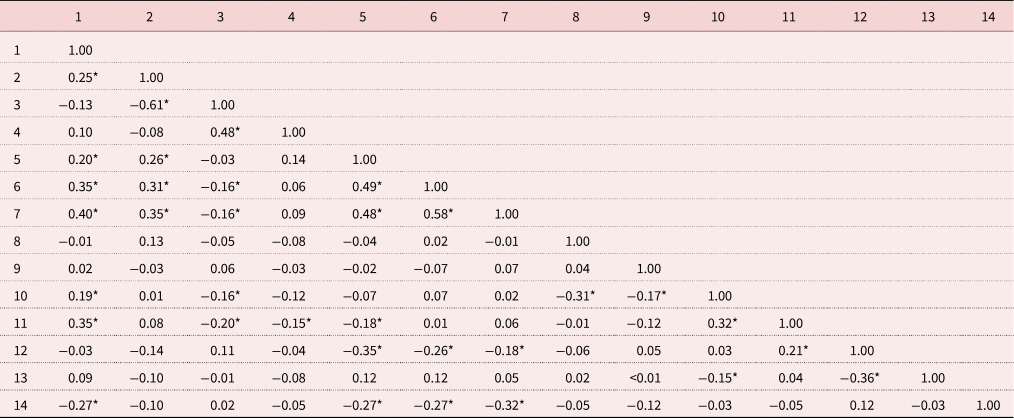
Notes: Values are Pearson correlation coefficients. 1 = efficacy, 2 = satisfaction, 3 = burnout, 4 = secondary trauma, 5 = knowing the person, 6 = comfort care, 7 = support for relationships, 8 = years of work in long-term care, 9 = female gender, 10 = university degree, 11 = professional staff, 12 = non-profit facility, 13 = small facility, 14 = involved in care planning (higher values associated with lower involvement).
Significance level: * p < 0.05.
Knowing the person
As we proceeded to the regression modelling, we first fit the full model to the Knowing the Person subscale. Standardised regression coefficients, reported in Table 3, show that the following variables were associated with attention to residents' personhood (p < 0.05): professional occupation, involvement in care planning, facility profit status, compassion satisfaction and self-efficacy. Burnout, trauma, facility size and most employee demographic variables (gender, years of work in LTC, university education) did not show statistically significant positive associations with the dependent variable knowing the person (p > 0.05). Overall, the model explained 29 per cent of the variance in knowing the person, and this is a large effect.
Table 3. Standardised regression coefficients (β) for three dependent variables
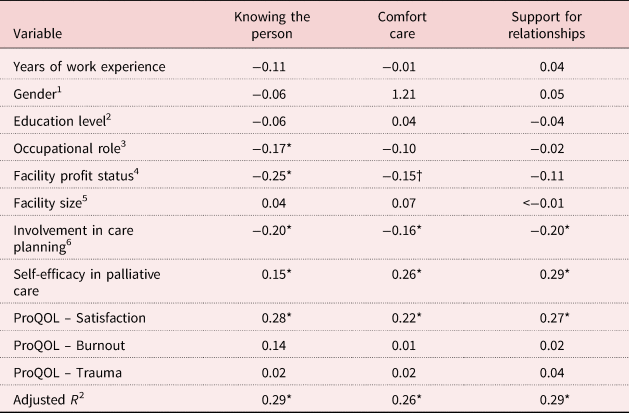
Notes: N = 183. 1. Woman = 1, other/not disclosed = 0. 2. University degree = 1, no degree = 0. 3. Professional/therapy (e.g. practical nurse, physiotherapist) = 1, supporting staff (e.g. care assistant, physiotherapy assistant) = 0. 4. Non-profit = 1, for profit = 0. 5. Small = 1, medium or large = 0. 6. Involved = 1, not involved = 2. ProQOL: Professional Quality of Life scale.
Significance levels: † p < 0.10, * p < 0.05.
We then compared restricted models to the full model (see Table 4). First, we compared a model excluding Block 1 (background characteristics) to the full model. There was no significant change in R 2, FΔ(4, 172) = 1.06, p > 0.05. Then we compared a model excluding Block 2 (organisational qualities) to the full model. In this case, there was a significant change in R 2, FΔ(2, 172) = 7.80, p < 0.05. A comparison restricting Block 3 (involvement in care planning) also resulted in a statistically significant change in R 2, FΔ(1, 172) = 8.19, p < 0.05. A comparison between Block 4 (employee wellbeing) and the full model resulted in statistically significant change in R 2 too, FΔ(3, 172) = 3.60, p < 0.05, as did a comparison involving Block 5 (self-efficacy), FΔ(1, 172) = 4.09, p < 0.05.
Table 4. Change in adjusted R 2 for regression models for three dependent variables
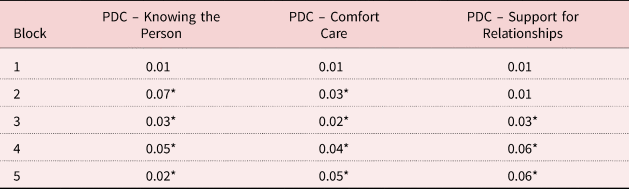
Notes: N = 183. PDC: Person-Directed Care scale. Block 1 included employee demographic variables (i.e. years of work experience, gender, level of education, occupation). Block 2 included organisational factors (i.e. facility size, facility profit status). Block 3 included engagement in team planning (i.e. involvement in care planning). Block 4 included employee wellbeing (i.e. three Professional Quality of Life subscales). Block 5 included palliative care self-efficacy (i.e. End-of-Life Professional Caregiver Survey scale).
Significance level: * p < 0.05.
Findings from both the full model and the backward stepwise regression models were generally consistent with hypotheses, with the exception that gender and facility size were not significant predictors of knowing the person in this sample, and that compassion satisfaction was the only domain of employee wellbeing that predicted knowing the person. The backward stepwise regression model indicated that while facility profit status was the most important predictor of knowing the person (consistent with hypotheses), employee wellbeing was a more important predictor than non-hierarchical distribution of work roles (i.e. engagement in care planning), which was contrary to expectation.
Comfort care
An additional model was constructed to understand predictors of comfort care. We first fit the full model to the Comfort Care subscale. Standardised regression coefficients, reported in Table 3, show that the following variables were associated with attention to residents' personhood (p < 0.05): involvement in care planning, compassion satisfaction and self-efficacy. Burnout, trauma, professional occupation, facility size and employee demographic variables (gender, years of work in LTC, university education, occupational role) did not show statistically significant positive associations with the dependent variable comfort care (p > 0.05). Facility profit status also did not show a statistically significant positive association with the dependent variable at the established level of statistical significance (i.e. p < 0.10). Overall, the model explained 26 per cent of the variance in comfort care, and this is a large effect.
Next, we compared restricted models to the full model (see Table 4). When we excluded Block 1, background characteristics, there was no significant change in R 2, FΔ(4, 172) = 0.77, p > 0.05. In contrast, restricting Block 2 (organisational qualities) did result in a significant change in R 2, FΔ(2, 172) = 3.78, p < 0.05. Restricting Block 3 (involvement in care planning) also resulted in a statistically significant change in R 2, FΔ(1, 172) = 5.56, p < 0.05, and the same was true of Block 4 (employee wellbeing), FΔ(3, 172) = 3.16, p < 0.05. Finally, a comparison involving Block 5 (self-efficacy) also resulted in statistically significant change in R 2, FΔ(1, 172) = 11.27, p < 0.05.
As with the regression model for knowing the person, while many of the findings from both the full model and the backward stepwise regression models for comfort care were consistent with hypotheses, others were not. For example, gender was not a significant predictor of comfort care; nor were facility size and profit status; furthermore, compassion satisfaction was the only domain of employee wellbeing that predicted person-centred palliative care. Contrary to expectation, the backward stepwise regression models indicated that certain employee characteristics, such as palliative care self-efficacy and compassion satisfaction, were more important predictors of comfort care provision than organisational variables.
Support for relationships
When we fit the full model to the Support for Relationships subscale (for details, see Table 3), the variables and involvement in care planning, compassion satisfaction and self-efficacy showed a statistically significant positive association (p < 0.05). In contrast, burnout, trauma, organisational variables (facility size and profit status) and demographic variables (gender, education, occupation, years of experience) were not associated with providing support for residents' relationships (p > 0.05). Overall, the model explained 29 per cent of the variance in support for relationships, and this is a large effect.
In further examining how well specific blocks of variables predicted support for relationships, an initial comparison, involving a restricted model that excluded Block 1 (background characteristics), did not result in a significant change in R 2, FΔ(4, 172) = 0.48, p > 0.05. The next comparison, for Block 2 (organisational qualities), also did not result in a significant change in R 2, FΔ(2, 172) = 1.40, p > 0.05. The third comparison, for Block 3 (involvement in care planning), did result in a statistically significant change in R 2, FΔ(1, 172) = 8.37, p < 0.05. An additional comparison, for Block 4 (employee wellbeing), also resulted in a statistically significant change in R 2, FΔ(3, 172) = 4.49, p < 0.05. Finally, a comparison for Block 5 (self-efficacy) resulted in a statistically significant change in R 2, FΔ(1, 172) = 14.76, p < 0.05 (see Table 4).
While many of the findings from both the full model and the backward stepwise regression models were consistent with hypotheses, contrary to expectation, gender, facility size and profit status were not significant predictors of support for relationships, and compassion satisfaction was the only domain of employee wellbeing that predicted person-centred palliative care. Contrary to expectation, certain employee characteristics (palliative care self-efficacy and compassion satisfaction) were more important predictors of comfort care provision than organisational variables, including a non-hierarchical distribution in work (i.e. engagement in care planning).
Discussion
In this study, we evaluated the relative contributions of organisational and personal qualities to aspects of person-centred care that are important to palliative care in LTC. Specifically, we examined the relative contributions of five variable groupings to three aspects of palliative care provision: comfort care, knowing the person and supporting relationships. The five variable groupings were: employee demographic variables (years of work experience, gender, level of education and occupation); organisational factors (facility size and facility profit status); occupational factors (involvement in care planning); employee wellbeing (compassion satisfaction, burnout and secondary traumatic stress); and palliative care self-efficacy. Overall, we found that occupational factors (involvement in care planning), employee wellbeing (compassion satisfaction and self-efficacy) and self-efficacy were each reliably associated with all measured aspects of person-centred palliative care. In contrast, facility size was not associated with person-centred palliative care, and facility profit status was associated only with efforts to know the person. Furthermore, employee background characteristics (gender, work experience and education level) and poor wellbeing (burnout and trauma) were not reliably associated with any of the outcome variables. These results raise the possibility that humanistic care is less related to intrinsic characteristics of health-care employees and more related to workplace factors, or to the kinds of personal factors that can be cultivated within the workplace, such as meaningful role engagement, compassion and self-efficacy.
Overall, self-efficacy and employee wellbeing (particularly compassion satisfaction) accounted for about one-third of the variance in person-centred care explained by the three models. Since compassion satisfaction and self-efficacy are both outcomes that can be cultivated, this finding offers important insight into strengthening person-centredness within a palliative approach in LTC. Many LTC facilities have not yet fully embraced a palliative approach to care despite supporting a great number of deaths (e.g. 30% per year in Canadian LTC facilities). Since employees who work in palliative care contexts say that reflecting on death can enhance their experience of work (Ablett and Jones, Reference Ablett and Jones2007; Sinclair, Reference Sinclair2011), shifting more explicitly towards a palliative approach might be one way for employers to nurture compassion satisfaction in a way that reflects the experiences of their employees. Other potential approaches include mission-centred hiring and organisation of work, and strong leadership (Drury et al., Reference Drury, Craigie, Francis, Aoun and Hegney2014; Kelly and Todd, Reference Kelly and Todd2017, Munroe et al., Reference Munroe, Morse and Price2020).
Self-efficacy, which showed a relationship to all three measures of person-centred care in this study, generally has a strong relationship with work performance (Stajkovic and Luthans, Reference Stajkovic and Luthans1998) and is very responsive to organisational ‘inputs’. For instance, it is known to be shaped by experience (Simons et al., Reference Simons, An and Bonifas2016), education (Ngo and Murphy, Reference Ngo and Murphy2005; Phillips et al., Reference Phillips, Salamonson and Davidson2011; Moir et al., Reference Moir, Roberts, Martz, Perry and Tivis2015) and empowerment (Manojlovich, Reference Manojlovich2005a, Reference Manojlovich2005b), which are all inputs that employers can provide. In this study, however, there was no correlation between years of work and palliative care self-efficacy, suggesting that self-efficacy in this domain does not increase automatically with experience in LTC. This suggests that a more direct focus on education and employee engagement is important for improving palliative care self-efficacy in this sector. In this study, involvement in care planning was associated with palliative care self-efficacy. In LTC, resident and family care conferences provide an important mechanism for communication about how well the approach to care is meeting the resident's and family's needs, and these results point to care conferences as a focus for palliative care quality improvement efforts. In our study, having a university degree and being in a professional role were also associated with efficacy, suggesting that external inputs such as education do help to promote efficacy. There are ongoing questions about how this education is best delivered in LTC, with some good preliminary results for on-the-job practical training. For example, one study showed that engaging care assistants in experiential learning through job shadowing in hospice care was an effective strategy to improve palliative care self-efficacy in LTC (Kaasalainen et al., Reference Kaasalainen, Brazil and Kelley2012). Additionally, several current initiatives focus on tailoring palliative education to the LTC context, and on communicating models of palliative care that are well-adapted to this sector and engage employees at all levels in the work (e.g. Van den Block et al., Reference Van den Block, Honinx, Pivodic, Miranda, Onwuteaka-Philipsen, van Hout, Pasman, Oosterverld-Vlug, Ten Koppel, Piers, Van Den Noortgate, Engels, Vernooij-Dassen, Hockley, Froggatt, Payne, Szczerbińska, Kylänen, Gambassi, Pautex, Bassal, De Buysser, Deliens and Smets2020).
Direct engagement in care planning accounted for about one-tenth of the variance in person-centred care accounted for by the three models and showed small- to moderate-sized correlations with knowing the person, comfort care and support for relationships. Since engagement in care planning was not associated with a higher level of education or having a professional role, it might be the case that engaging team members directly in care planning, regardless of their education level or role, helps to cultivate person-centred attributes, including more active consideration of their knowledge of the resident, what would promote the resident's comfort and what support the resident needs to participate successfully in the family. The finding that care planning was not associated with a higher level of education is promising, as the active engagement of all team members in supporting the resident's care plan is very consistent with a palliative approach to care, which typically advocates for inter-disciplinary teamwork and role flexibility (Van der Steen et al., Reference Van der Steen, Radbruch, Hertogh, De Boer, Hughes, Larkin, Francke, Jünger, Gove, Firth, Koopmans and Volicer2014; World Health Organization, 2021).
Other variables were less reliably associated with the aspects of person-centred care that we studied. For instance, in the full regression models, occupational role was associated only with knowing the person, and t-tests comparing those in professional roles to those in supporting roles showed that support staff such as care assistants reported stronger levels of person-centred care than professional staff. As 80–90 per cent of direct resident care is provided by care assistants, they spend more time with residents and are responsible for most interpersonal interactions between residents and staff (Caspar et al., Reference Caspar, Le and McGilton2019; Abrahamson et al., Reference Abrahamson, Fox, Roundtree and Farris2020). Care assistants value the relationship aspect of their role and adjust their care based on the knowledge of the person (Canham et al., Reference Canham, Battersby, Fang, Sixsmith, Woolrych and Sixsmith2017; Abrahamson et al., Reference Abrahamson, Fox, Roundtree and Farris2020). Professional staff also value relationships with residents, but current staffing levels in Canadian contexts place professional staff in treatment, consulting or managerial roles, and this removes them from the bedside and limits their ability to know the resident with the same degree of intimacy as care assistants (McGilton et al., Reference McGilton, Boscart, Brown and Bowers2014).
We also noticed that even though experiences of burnout and secondary traumatic stress were not important predictors of palliative care provision in this sample, those in supporting roles, such as care assistants, were more likely to report more of these symptoms than those in professional roles, such as nurses. Although this finding was correlational, a long tradition of research on stress suggests that those whose work positions hold less status are likely to be more vulnerable to stress (e.g. Singh-Manoux et al., Reference Singh-Manoux, Adler and Marmot2003; Thompson et al., Reference Thompson, Gaglani, Naleway, Thaker and Ball2014). Reports about the Canadian LTC context document that support staff in LTC are often people who also experience social stigma in their daily lives related to gender, ethnicity and class dynamics in Canadian society, raising questions about whether factors outside the organisation might be operating as a hidden ‘third variable’ in the observed relationship between occupational role and burnout or secondary traumatic stress (Shutes and Walsh, Reference Shutes and Walsh2012; Estabrooks et al., Reference Estabrooks, Squires, Carleton, Cummings and Norton2015). On the other hand, the Canadian LTC sector may be more hierarchically oriented than in other nations (Banerjee et al., Reference Banerjee, Armstrong, Armstrong and Rosenau2011), which suggests that the organisational structure of LTC could also be contributing to the observed association. We were encouraged to see that on average, scores on measures of burnout and traumatic stress fell well below the threshold for concern, and this was true for both professional and support staff. To the extent the reasons for the observed relationship lie within the organisation, it is possible that implementing a palliative approach to care, which emphasises a strong and flexible team approach, and includes planning for the potentially stressful experience of death, and addressing loss openly, might help to decrease burnout and secondary traumatic stress for all employees.
We also found that facility size had no bearing on person-centred palliative care in this study. In fact, surprisingly, despite literature suggesting that for-profit status is a disadvantage to high-quality care, and that it is challenging to cultivate a change in culture within large organisations (Sterns et al., Reference Sterns, Miller and Allen2010), in our results, for-profit facility status was associated with knowing the person. This may be an anomalous result reflecting potentially unique qualities of the single non-profit organisation or the ‘umbrella’ for-profit organisation that participated in this study. Nevertheless, one related descriptive finding deserves additional consideration. That is, occupational comparisons showed that support staff tend to express greater adaptation of care to their knowledge of the person. If for-profit homes have a higher ratio of support staff to professional staff, they may have shown a greater advantage for this reason. Nevertheless, this would not explain the association between for-profit status and comfort care, as professional and support staff showed no significant differences on this variable. Larger-scale surveys, inclusive of multiple sites with different business models, would be most helpful for understanding whether and how facility size and profit status matter to person-centred palliative care. Overall, our results offer hope that person-centred care can be cultivated even within large organisations. To better study the role of facility size and occupation in the delivery of person-centred palliative care, larger, multi-organisational studies will be needed.
The significance of this research also rests in what was not observed. In advancing efforts to improve person-centred palliative care in LTC, there is a risk of assuming that individual employees are responsible for deficits in person-centred care. In this study, employee factors such as years of work, education and gender had relatively little association with person-centred care. In the past, there has been a great deal of focus on looking to employee characteristics rather than organisational features to understand care shortcomings (cf. Kearney and Weininger, Reference Kearney, Weininger and Hutchinson2011). The variables most reliably associated with a person-centred palliative approach to care in this study were ones that can be shaped by the workplace, including self-efficacy, compassion satisfaction and involvement in care planning. As palliative approaches continue to develop within LTC, leaders can acknowledge these findings by engaging team members at all levels in the work, cultivating skills and self-efficacy for palliative care, and helping employees to reap the benefits of providing better support to residents who are approaching the end of life, along with their families.
Strengths and limitations
This study is one of very few to have considered the relative importance of individual and organisational factors to person-centred care delivery in the LTC sector. Nevertheless, given its reliance on a sample drawn from an intervention study, it has some limitations. First, it encompasses two groups that performed differently on some of the measures included in the study. These groups of professional and supporting staff were primarily comprised of nurses and nursing care assistants. Based on our results, it will be important to distinguish these two groups in future research on this subject. Secondly, the reliability of our examination of organisational factors is limited by our inclusion of a small number of homes. Although our results are statistically significant, suggesting the reliability of the finding that organisational factors are more important than personal ones, some of the findings were in a direction opposite to expectations, and this might be accounted for by particular qualities of the four homes included in this study. Model overfitting can also be a concern when a regression model has too many parameters for the sample size or the model is too closely based on unique characteristics of the sample. In this case, the number of parameters is balanced with the sample size, but there is some uncertainty about whether unique characteristics of the sample have determined some of the results. Therefore, these results should be considered preliminary and used to inform the design and interpretation of future research.
Conclusion
This study examined the association between a number of employee and organisational factors and three facets of person-centred palliative care. We found that one job characteristic, involvement in care planning, was reliably associated with person-centred palliative care. We also found that two modifiable personal characteristics, self-efficacy and compassion satisfaction, were associated with person-centred palliative care. Our results also suggested that neither facility size nor some employee characteristics (gender, work experience and education) were reliable predictors of person-centred care. We conclude that it is reasonable for LTC facilities that would like to improve person-centred palliative care to consider ways to further cultivate employees' self-efficacy and compassion satisfaction.
Author contributions
PVH, LM, SK, TS, GT, LV and AW-G co-designed the survey and oversaw data collection. PVH planned and conducted the analysis in consultation with LM. PVH wrote the initial draft of the manuscript and all authors edited the manuscript. PVH formatted the manuscript for publication. PVH is guarantor. All authors read and approved the final manuscript.
Financial support
This work was supported by a Canadian Institutes for Health Research Partnerships for Health Systems Improvement grant.
Conflict of interest
The authors declare no conflicts of interest.
Ethical standards
The study protocol was reviewed and approved by seven university-affiliated or integrated ethics boards (Hamilton Integrated Research Ethics Board, No. 0427; Brock University, No. 15-102; McGill University, No. 281-1214; University of Saskatchewan, No. 15-270; University of Regina, No. 15-190; University of Manitoba, No. H2015:374; University of Calgary, No. 15-2277) and by local health authorities or organisations as required. Study participants reviewed an information form that reviewed all known requirements, risks and benefits associated with participating. Choosing to proceed with the survey implied free, informed consent.








