Over recent years, British psychiatry has experienced difficulties with the recruitment and retention of practitioners (Reference Kendell and PearceKendell & Pearce, 1997; Reference PiddPidd, 2003). From the Royal College of Psychiatrists’ 2004 census it may be estimated that 2–4% of consultant posts are currently vacant (the proportion would rise considerably if posts filled by locum consultants were counted as unfilled) (Royal College of Psychiatrists, 2005).
Studies suggest that there is a much more fundamental crisis in psychiatry. Whereas sixth-form (final-year) school students often express an active interest in, and even a preference for, psychiatry as a potential career, their attitude changes during their time at medical school (Reference Maidment, Livingston and KatonaMaidment et al, 2003). Medical students who are interested in the broad psychosocial aspects of care in their early careers appear to lose interest in these areas as graduation approaches (Reference Feifel, Moutier and SwerdlowFeifel et al, 1999). Medical students in one British survey viewed psychiatry as the least desired clinical specialty in which to make their career (Reference Rajagopal, Rehill and GodfreyRajagopal et al, 2004), a situation broadly reflected in other countries (Reference Abramowitz and Bentov-GofritAbramowitz & Bentov-Gofrit, 2005). One factor that was particularly highly correlated with the choice of a career in psychiatry was the subjective experience of the specialty as a medical student (Reference Goldacre, Turner and FazelGoldacre et al, 2005).
In this article we explain how clinical placements can be used to attract students into psychiatry, focusing on practical and modern methods for clinicians who find themselves in the role of teacher.
Is it our duty to teach medical students?
In the UK, many consultant psychiatrists are expected to provide clinical placements for students from local medical schools, with remuneration via service increments for teaching (SIFT) payments to their employing National Health Service (NHS) trust. According to General Medical Council (GMC) guidance, it is imperative that all doctors have the ability to teach effectively (General Medical Council, 2002) and many consultants will have teaching commitments included in their new contracts under the section ‘supporting professional activities’. Although not all clinicians will feel the need to learn how to teach more effectively in a clinical setting, recent political changes have meant that this will become increasingly uncommon. Since the publication of Modernising Medical Careers (Modernising Medical Careers & UK Clinical Research Collaboration, 2005), the medical Royal Colleges and Department of Health have emphasised good teaching skills within the core competencies of the requirements of all qualified doctors (Box 1).
Box 1 Guidelines on expected teaching and training skills for all doctors
Doctors should be able to demonstrate that:
-
• they have the knowledge, skills and attitudes to undertake a teaching role
-
• they can set educational objectives, identify learning needs and apply teaching methods appropriately
-
• they can use opportunities for teaching
-
• they can communicate and share information on a one-to-one basis and in small groups
-
• they can give as well as seek feedback
-
• they have the willingness, enthusiasm and patience to teach
(Adapted from the Foundation Committee of the Academy of Royal Colleges, 2005)
Clinicians in many areas are now being encouraged to gain teaching qualifications through courses approved by the Higher Education Academy (HEA) (Reference El-Sayeh, Waller and BuddEl-Sayeh et al, 2005). In addition, recent expansion in the number of medical school places means that an ever-larger pool of clinical placements is required.
Aside from the logistical requirements, there is also an ethical argument for teaching effectively. It could be reasoned that we owe our patients a moral duty to teach medical students the basic psychiatry that any registered doctor should know. Not doing so could be seen as a betrayal of our obligation to a future generation of patients and carers alike.
There are many reasons why psychiatrists should learn to teach medical students and virtually no good reasons why they should not (Box 2).
Box 2 Advantages and disadvantages of learning to teach undergraduates effectively
Advantages
-
• It increases your value to local NHS organisations, employers and patients
-
• It enhances confidence and self-esteem
-
• It may improve students’ learning and future recruitment into psychiatry
-
• It provides a different role aside from basic service provision or management
-
• It counts towards professional development and CPD activities
-
• It provides personal satisfaction in watching others learn and should keep you up to date with advances in psychiatry
-
• Teaching skills can be generalisable and used in other settings, such as teaching postgraduates or allied healthcare professionals (Reference Dahlstrom, Dorai-Raj and McGillDahlstrom et al, 2005)
Disadvantages
-
• Reduced time available for other clinical activities
-
• Relative lack of support and recognition from employing organisation and peers
-
• Limited resources for learning to teach (space, money, facilities, information technology)
-
• Increased workload: learning to teach effectively can be hard work
Where to learn how to teach
There are several practical ways in which to improve clinical teaching skills and the methods chosen will largely depend on your own interest and enthusiasm for teaching (Box 3).
Box 3 Practical ways to improve teaching skills in psychiatry
• Read
The ABC of Learning and Teaching in Medicine (Reference Cantillon, Wood and HutchinsonCantillon et al, 2003)
Medical Education (journal) http://www.mededuc.com/
Medical Teacher (journal) http://www.medicalteacher.org/
• Access internet resources
Higher Education Academy: http://www.medev.heacademy.ac.uk
University of Dundee Centre for Medical Education: http://www.dundee.ac.uk/meded/frames/home.html
University of Medicine and Dentistry of New Jersey Center for Teaching Excellence: http://cte.umdnj.edu/
• Attend local teaching refresher courses organised by the university or deanery
• Attend local HEA-approved long courses
• Register with a distance learning course in medical education
Dundee Centre for Medical Education offers Certificate to Masters level qualifications in medical education
University of Cardiff offers Diploma and Masters qualifications
University of Bristol offers Certificate to Masters courses
At a basic level, clinicians could access popular journals and internet-based resources, which may or may not be education-specific. These often give advice on teaching methods and examples of best practices in medical education.
There may be local educational courses, often organised by the local deanery or a university medical education unit. Most courses act as basic refresher sessions in which participants are taught a few readily learned skills.
However, trying to improve your teaching skills by attending a few sporadic ‘events’ is unlikely to result in sustained improvement. It is rather like expecting more difficult patients to improve after one meeting with a psychotherapist.
At a more advanced level, courses are likely to be more substantial and may require the completion of practical assignments and essays. These are often run in conjunction with university teaching and learning departments, and may lead to a postgraduate qualification in education. Such courses are probably more geared towards clinicians with an academic role, or those acting as local clinical tutors, and if all you do is teach the occasional medical student this could be seen as using a sledge hammer to crack a nut!
In the middle ground between the day course and the substantive course is participation in a peer-led teaching network. The Joint Information Systems Committee (JISC) runs an e-mail discussion group for medical education (http://www.jiscmail.ac.uk/), and the Higher Education Academy subject centre covering medicine maintains a list of online resources and discussion forums (http://www.medev.heacademy.ac.uk/).
Those who are wary of the internet or who want to meet people involved in teaching in their local area might prefer to participate in pioneering projects set up in some cities in the UK. In an earlier APT article Reference Vassilas, Brown and WallVassilas et al(2003) described how such a network improved the teaching ability of all grades of psychiatrist in the West Midlands region.
Finally, you could consider taking a medical teaching course on a distance-learning basis, an option probably more suited to those clinicians with a specific interest in medical education. Distance learning is particularly suitable for busy clinicians whose duties make it difficult to attend local courses regularly and those who feel more comfortable with internet-based learning and lone study.
How can we give students a positive experience of psychiatry?
The answer to this question is probably fundamental to why you yourself chose a career in psychiatry. It was probably not the hours spent in a library reading a ‘stodgy’ psychiatry text that piqued your interest. More likely, it was a particularly charismatic tutor or interesting patient that initially drew your attention to this fascinating and varied specialty. It is surely the recreation of this same traditional learning environment and sets of experiences – coupled with more modern learning theory – that will prove effective in teaching psychiatry in the future.
How most clinicians teach
To enable us to explain particular teaching methods more effectively, we will first discuss how students are currently taught and learn.
Most psychiatry and psychiatry teaching is experienced while the student is in an NHS clinical setting, not in a university lecture theatre. Owing to recent changes in the NHS, including altered working patterns for junior doctors, it is likely that a greater role in undergraduate teaching will fall to senior staff. Unfortunately, most senior clinicians are ‘willing amateurs’ with regard to modern teaching methods. Few will have had specific training, and the majority will have learnt their educational methods through a ‘see one, do one, teach one’ apprenticeship model (Reference El-Sayeh, Waller and BuddEl-Sayeh et al, 2005). Most of their practical clinical teaching will occur on wards, in clinic rooms or in the community and will involve between one and three students at a time. This will therefore be the focus of the following practical guidance.
How most students learn
Modelling
There are many theories of how students learn (Box 4). The process of modelling may be particularly effective in teaching attitudes and skills. The teaching clinician should aim not just to be, but also to be seen to be, a suitable role model for students. Psychiatrists should appear as skilled, modern NHS professionals working effectively with patients, carers and teams to provide the best available evidence-based care in a challenging and dynamic field. Experience tells us that nothing will do more to dull a student’s initial interest than teachers who are either disinterested, distant or take a cavalier approach to teaching.
Box 4 Strategies important in student learning
-
• Modelling another’s behaviour
-
• Deep v. surface learning
-
• Experiential learning
-
• A balanced VARK profile
Deep v. surface learning
The approach that students take may involve deep or surface learning. These concepts are discussed in some detail by Reference Curran and BowieCurran & Bowie (1998).Footnote 1 Essentially, surface learning is associated with memorising, is often poorly retained and may be driven more by the need to satisfy short-term outcomes such as passing an examination. Deep learning depends on understanding underlying theories and concepts and their practical application, and it is more likely to be retained and applied in different situations.
Teaching that focuses on ‘spoon-feeding’ and has a heavy factual content is more likely to result in surface learning. Alternatively, sessions that encourage exploration and discussion of underlying concepts as well as allowing students to apply these theories in clinical practice may help nurture deeper learning.
Experiential learning
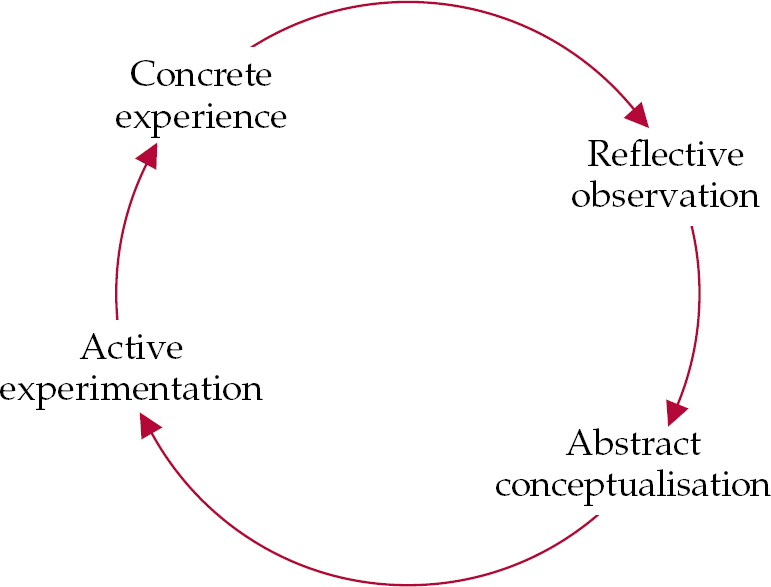
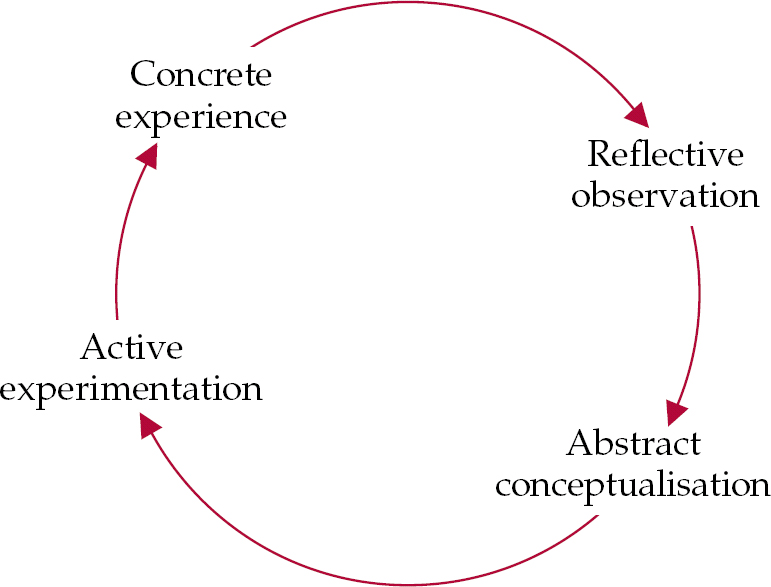
Another model that is valuable in understanding student learning is the experiential learning cycle, which may be crucial in helping to encourage the deep-learning process.
Experiential learning theory states that learning is most effective when based on direct experience (Reference KolbKolb, 1984). Experiential learning should be the staple of medical training and it is a process similar to that expected of active practitioners engaged in lifelong learning. It involves a cycle in which learners become engaged in a new experience, which should lead to a process of reflection, using feedback from various sources, including tutors. Learners must then be able to formulate and process these new ideas into sound and logical theories, which can be used abstractly and applied to completely new situations, hence completing the cycle (Fig. 1).
The VARK model
As individuals, we tend to favour certain sensory modes for learning information. Reference Fleming, Zelmer and ZelmerFleming (1995) identified the key styles as visual, aural, read/write and kinaesthetic (VARK), and the VARK model of teaching uses the medium to help transfer the message. Thus, the medium used by the teacher (e.g. visual teaching) should ideally match that preferred by the student (e.g. visual learning). This match in preferences may make the resultant learning experience more productive.
Much teaching on wards is auditory or kinaesthetic (i.e. what is said and physically performed), and it is important not to forget to use visual or reading materials as part of a broader teaching strategy.
It may be helpful to understand one’s own preferred learning and teaching styles, as this may identify an overreliance on a particular medium during teaching. Being aware of current practices may help to broaden the repertoire of media in which you teach, and hence reduce the chances of being ineffective with students whose VARK profile differs greatly from your own. You can identify your own preferred learning, and hence teaching, strategies from the VARK questionnaire (Reference FlemingFleming, 2006).
Teaching in different environments
House rules
Attend to basic needs
Certain basic rules apply to all teaching of medical students (Box 5). Before embarking on teaching new students, tutors should try to ensure that the needs of their charges are met at the lower levels of Maslow’s hierarchy of needs (Reference MaslowMaslow, 1943). Students that do not have adequate accommodation and access to transport, canteens or food are less likely to be fully focused on learning. Making basic enquiries about these issues also helps create a positive first impression, which will enhance the ensuing learning relationship. Tutors must also not forget that pastoral issues may arise that affect a student’s attendance or performance (see below).
Box 5 House rules
-
• Ensure that basic, ‘non-clinical’ student requirements are addressed
-
• Take time to create a positive learning environment prior to a placement
-
• Early dialogue is useful to clarify student and tutor requirements
-
• Encourage other stakeholders to become involved in teaching processes
-
• Promote self-directed, active learning
Prepare the learning environment
Try to find time to create a good learning environment before the student arrives. This may involve alerting clerical or clinical teams that a student will be attached to the team for a given period and highlighting the reasonable expectations that this individual may have of them during this time. For example, it may be agreed that clinical staff should identify suitable patients for the student to interview, or that the team secretary may be involved in arranging for the student to have up-to-date clinical timetables. Familiarising yourself with the medical schools’ student learning objectives and other teaching materials will allow your teaching to be more focused on the student’s needs and possibly less driven by your personal views on what you regard as important to student learning.
Contact the student
Always attempt to contact the student either before the placement begins or very early into it. As well as clarifying your availability to teach, it allows you to state your expectations of the student. This may involve listing clinics that should be attended or simply explaining local protocols and procedures. Preparation before the beginning of a placement can minimise confusion and misunderstanding as time progresses.
Involve others
Strive to optimise your time and teaching opportunities by allowing (or persuading) other stakeholders to become involved in the student’s learning. In view of the greater user and carer involvement in the NHS, patients should be included in the planning and delivery of teaching, in line with the recommended partnership approach. Simple courtesies such as gaining the patient’s consent to be seen by a student (before the student arrives) and explaining the purpose of the teaching session and the importance of confidentiality to students and patients alike should be basic requirements. Active involvement of suitable patients and carers in teaching is also recommended (Reference FarrellFarrell, 2004). You might ask the student to talk to carers about their subjective experiences, and your own time might be usefully spent asking patients about their involvement in teaching or their opinions of the student’s communication skills. Likewise, aim to create a ‘non-consultant focused’ teaching model by asking medical colleagues such as senior trainees and staff and associate specialist (SAS) grade doctors, as well as non-medical staff, to take part in teaching or to provide clinical experiences. The student could spend time on duty with a community psychiatric nurse, or observe a junior doctor on call. This process is important in allowing the student a more balanced and realistic learning environment as well as conserving your own time and resources.
Encourage active, self-directed learning
Promote active rather than passive learning. Students who are goal-directed and active in their approach to learning are more likely to acquire lasting skills and knowledge. In addition, an active approach is fundamental to the process of experiential learning (see earlier). Practical aspects to encourage active learning are discussed in further detail below.
Encourage self-directed learning. This does not mean simply telling students to devote long periods to reading in the library; they should also spend time on more practical skills. For example, asking a student to perform specific tasks between sessions, such as reading up on a particular topic before making a presentation, or drafting a patient discharge letter or even a patient information leaflet, can add to their clinical experiences without an overreliance on staff time.
Teaching on psychiatric wards
Formal ward rounds in which a clinical team visits patients’ bedsides, examines the patients and reviews their progress, although commonplace in other medical specialties, are a rarity in modern British psychiatry (students are initially often surprised by this fact). During a clinical ward round, psychiatric patients are often invited to take part in the planning of their care. The pressure of time, the lengthy discussion of multiple agendas and the often difficult physical environment (excessive noise, lack of space) can be detrimental to learning (and teaching). Ward rounds are thus rarely the most suitable teaching arenas.
The student’s role in ward rounds has often been primarily passive and undirected, and was seen as a hindrance to the main clinical proceedings. During rounds, students may have been offered occasional pearls of clinical wisdom, may have been critically examined before other members of the clinical team or, worse still, may have been completely overlooked. Modern teaching and learning in ward rounds should be quite the opposite, i.e. active and goal-directed and students should be seen as playing a useful role in the clinical team. Box 6 gives some tips on how to make best use of the teaching opportunities presented by the ward round.
Box 6 Tips for teaching on psychiatric ward rounds
-
• At a regular interval (once weekly, if possible) dedicate a ward round to teaching
-
• Be selective about each student’s role in a ward round: it is rarely necessary for them to attend all of every round – they could be asked to attend the parts that are relevant to ‘their own’ patients (as are nursing staff)
-
• Ensure that students have been allocated a patient or patients for whom they are ‘responsible’ and whom they follow from admission to discharge
-
• Make sure that one suitable clinician is specifically allocated to teach the student during the round
-
• Ask students to perform tasks during the round, e.g. presenting a patient’s case or progress, or summarising the views of the carers/other stakeholders through suitable information-gathering
-
• Give students tasks between ward rounds, such as history-taking practice
-
• Allow time to discuss each student’s performance and issues such as management or ethical dilemmas during the round or during a supervision session
(Reference Murdoch Eaton and CottrellMurdoch Eaton & Cottrell, 1998)
Teaching in clinics
As with teaching on ward rounds, teaching in clinics, if done correctly (Box 7), can be effective within a challenging environment.
Box 7 Tips for teaching in clinics
-
• Book a light clinic to allow plenty of extra time for teaching
-
• Ask students to complete specific tasks during a consultation, such as writing down their observations or differential diagnoses
-
• ‘Hot-seat’ students by asking them to lead the consultation, and discuss their experience and findings with them afterwards
-
• Allow students to see patients on their own during a clinic and then present their findings to you (ensure, of course, that appropriate safeguards are in place)
Teaching in community or assertive outreach/crisis resolution teams
Most clinical teams are expected to provide out-patient services, and teaching in traditional community mental health teams utilises many of the generic skills used in teaching in clinics or on wards. However, changes in the way in which these teams operate may affect teaching provision. The past 5 years have seen a rapid expansion in new community teams, including assertive outreach and crisis resolution teams (Department of Health, 2004), and it is likely that increasing numbers of students will be attached to such teams as in-patient numbers continue to fall. These teams work solely in an out-patient or community setting, and students attached to them may have only this environment in which to learn psychiatry. This presents new challenges to both students and teachers, in terms of the types of patient (client) students are likely to meet, as well as the environment in which the teaching takes place.
Primarily, learning will be experienced ‘in the field’, and therefore the learning experiences must take this into account. Some will be opportunistic, but many can be prepared in advance (for example in prearranged home visits or assessments). As with teaching in clinics, clear objectives and an active student role will enhance the overall experience. Additional care must be taken when exposing students to situations or environments in which they might come to harm. Box 8 summarises tips specific to teaching in the community.
Box 8 Tips for teaching in the community or with assertive outreach/crisis resolution services
-
• Do not expose a student to situations that are inappropriate to their level of experience, e.g. interviewing patients unsupervised at home
-
• Ensure that the student has access to appropriate safety measures such as a mobile phone, break-away training and knowledge of hospital alarm systems
-
• Allow students to shadow on acute assessments where possible and to report back on the roles of the clinicians that they have observed
-
• Try to give students the opportunity to follow patients seen in on-call or emergency assessments through ensuing admission or treatment
-
• Make use of all teaching opportunities, for example by tutoring students while driving to an assessment or between on-call assessments
Although these settings are probably the most challenging in which to teach, they often provide students with the most well-remembered and gratifying experiences.
Teaching in psychiatric sub-specialties
The majority of medical students spend most of their psychiatric placement within a general adult or old age psychiatry setting. This is partly historical and partly because this environment is thought to provide the greatest variety of relevant clinical experiences for undergraduates. Some, however, will be placed in one of the many sub-specialties that have developed over the years. The teaching skills already discussed are generalisable to the sub-specialties, but students who gain all of their psychiatric experiences within a particular sub-specialty may have a rather skewed view of psychiatry. On the other hand, offering students an experience in a regional centre of excellence such as a local addiction unit or secure facility can be a potential strength as long as their overall experience is balanced.
A few practical steps that can be taken to help avoid these difficulties and enhance teaching are detailed in Box 9.
Box 9 Tips for teaching in psychiatric sub-specialties
-
• Emphasise areas that are generic to psychiatry (rather than specific to the sub-specialty) and directly relevant to the core skills required by the student. Be prepared to liaise with colleagues in other psychiatric specialties to ensure that your students get broader experiences
-
• Keep it short and simple (KISS) – don’t be tempted to teach too much detail on your particular specialty – and be guided by the overall course aims and objectives
-
• Stress areas of your specialty that may add value to their experience and create a lasting impression, for example a visit to a local specialist facility such as a regional secure unit in forensic psychiatry, or attendance at a family therapy session in child and adolescent psychiatry
-
• Take opportunities to teach students who come into contact with your team through ‘shared’ patients, for example undergraduates on a surgical firm whom you meet as a liaison psychiatrist, or students placed with an infectious diseases or liver unit team with whom you have contact as an addiction psychiatrist
Distance learning
As students on clinical placements are often based at some distance from the main academic centre, there is an increasing need to develop distance learning resources as part of modern courses. It is important, therefore, that students have suitable computer access during any clinical placement. Although local tutors are seldom involved in their students’ distance learning, there are a few aspects that you should be aware of, as the students’ learning tasks may have a direct bearing on the types of clinical experience that they seek.
At the University of Leeds, the School of Medicine dedicates a session to introducing undergraduates to the distance learning resources (e.g. online discussion rooms and self-assessment) available and giving them simple preparatory tasks such as making comments in a discussion room, viewing videos and completing internet searches for web-based materials. To explore the ‘virtual learning environment’ used in Leeds to teaching psychiatry go to the Bodington website (http://vle.leeds.ac.uk/site/nbodington/) and follow the links to ‘Faculty of Medicine & Health’ and ‘School of Medicine’.
Giving feedback
‘Students must receive regular and consistent information about their development and progress’ (General Medical Council, 2002: p. 13).
Giving quality feedback is a skill in its own right and needs to be learned. The reflective teacher should recall that receiving feedback is not easy. Giving it is much easier, particularly if it is negative. Feedback needs to be constructive and instructive, so that it is viewed not as criticism but as part of the learning process. It is important to provide the student with something on which to reflect and build using the experiential learning cycle, as this will reinforce good practice and promote deep learning. There are many dos and don’ts regarding feedback, and some key points are listed in Box 10.
Box 10 Some guidelines for giving feedback
-
• Arrange to give feedback as soon as possible after the session under review
-
• Give feedback throughout an attachment: do not leave it until the final assessment
-
• Before giving your views, ask the student to reflect on what went well during the session and on what they think could be improved
-
• Make sure that the first piece of feedback is positive: even if the student is particularly poor a good teacher should be able to find something good to say
-
• Provide the student with something on which to reflect and build using the experiential learning cycle: this will reinforce good practice and promote deep learning
-
• Avoid personal feedback, unless you have to address attitudes or professionalism
-
• Feedback should be practical and focus on core aspects of the student’s skills, behaviours and knowledge, not on minutiae
-
• Be honest
-
• Suggest areas or actions for improvement or frame your feedback so that the student can find their own solutions e.g. ‘Your background history lacks detail – how do you think you might get some additional information?’
-
• Always end on a positive note, encouraging the learner to reflect and continue on the learning cycle
(Reference Fullerton, Ketteridge, Marshall and FryFullerton, 2003; Reference GordonGordon, 2003; Royal College of Psychiatrists, 2004)
Although ‘it is better to give than to receive’, it is important that you have feedback on your performance as a teacher. This can come from a number of sources: yourself, peers and students. Feedback from oneself is a process of reflection, asking ‘How could I have done that better?’ Peers can provide valuable feedback and there are various systems and methods for peer review of teaching (Higher Education Academy, 2005). Feedback from students is also useful and easy to obtain: ask the student how they found a session, what they learned or what else they would like to know, or how the session might have been improved.
Problems and how to deal with them
Inappropriate attitudes
Dealing with difficulties related to attitudes and professional behaviour is an area fraught with potential problems. It is hard to reinforce the appropriate and ignore the disruptive behaviours. The professional behaviour of most students will be in line with what we as experienced clinicians and the GMC expects. However, a small number will display behaviours that will arouse strong negative emotions, including anger, hopelessness or even fear for patients. Given that medical students are adult learners with responsibility for their own learning and actions, neither the heavy-handed or the softly-softly approach may be beneficial. Feedback should be given along the lines described above, with reminders to the student of their professional responsibilities as laid out in both Tomorrow’s Doctors (General Medical Council, 2002: p. 3) and Good Psychiatric Practice (Royal College of Psychiatrists, 2004: pp. 43–44).
Non-attendance
Students should be asked and expected to communicate their reasons for absence, in advance if possible. Attendance difficulties can be viewed as an opportunity for the student to learn about working in a multidisciplinary team, with reminders of their responsibilities when they are employed as doctors. Frequent non-attendance should be queried with the student, and the responsible medical school department should be informed. Students should be advised that if they do not turn up, they may not gain sufficient clinical experience to be able to progress in their studies.
Lateness
Lateness may be unavoidable but the professional approach, as we use with our patients, is to apologise and explain the reasons for the delay. Students sometimes need to be reminded of this and they should be asked to reflect on how they might feel if a lecturer or tutor arrived late or did not turn up. Again, late attendance can be reframed as an opportunity for learning about professional attitudes and teamworking.
Dishonesty
‘All those who teach, supervise, counsel, employ or work with medical students have a responsibility to protect patients if they have concerns about a student. Where there are serious concerns … it is essential that steps are taken without delay to investigate the concerns to identify whether they are well-founded and to protect patients’ (General Medical Council, 2002: p. 17).
Honesty is considered a core attribute for a doctor. Students who do not tell the truth should be referred to the course manager and the relevant authorities at the medical school, as this is an issue that the GMC indicates should be raised as soon as possible.
Get the facts
Box 11 outlines how you should deal with problem students. The following fictitious accounts illustrate the importance of trying to establish why the student is ‘behaving badly’.
Box 11 How to deal with problems
Constructive feedback
-
• Give the student constructive, succinct and ‘improvement-focused’ feedback (Box 10)
-
• Try to find out what is causing the problem
-
• Get feedback on your own teaching
Non-attendance and lateness
-
• Stress the importance of the professional values of punctuality and attendance early on
-
• Set an example yourself and forewarn students of expected lateness and absence
-
• Record students’ regular absences or lateness
-
• Inform the medical school if the behaviour has a bearing on the student’s suitability to practise
Lack of honesty/disruption
-
• Explore the student’s (and other parties’) opinions on the problem
-
• Clarify any misunderstanding
-
• Take appropriate steps to ensure that disruption ceases and reconciliation is sought
-
• Inform the medical school if the behaviour has a bearing on the student’s suitability to practice
Pastoral issues
-
• Be aware of support structures and routes of referral available for students with difficulties, such as the university’s student counselling or health services
Example 1: Caught out
A student was on a placement split between sessions in primary care and psychiatry. The student failed to attend a session with the consultant psychiatrist without prior explanation. He later said he had been at a session arranged by the GP. There were concerns about his clinical skills and the GP phoned the psychiatrist to discuss their worries. The absence was mentioned and it transpired that the GP had not arranged a session as the student had claimed. When confronted with this evidence, the student made up further excuses. He was therefore referred to the course manager and subsequently to the Dean of the medical school for further action.
Example 2: An unexplained absence
A student had been absent from organised clinical teaching sessions for 3 days in a row. The supervising consultant was concerned and asked that the student be contacted by the medical secretary via their mobile telephone to ascertain their reasons. It transpired that the student’s mother had died earlier that week. The consultant contacted the medical school, which promptly arranged additional support for the remainder of the placement, including bereavement counselling and deadline extensions for outstanding coursework.
Pastoral issues
Although it is easy to forget, students have problems and worries other than learning and teaching issues related to psychiatry. It is important to be aware of pastoral issues and to know where to direct a student in the event of difficulties. Most students have a personal tutor and universities have student counselling services and medical centres. There are also online services and confidential helplines for students in most universities. One should not play the role of psychiatrist or doctor to the student, but know who to refer them to. If a problem is urgent or serious it may be appropriate to report it to the course management team. If you are concerned about a student’s health, dicuss this with the team as someone may well already be aware of the problem, particularly if it involves chronic or severe illnesses such as anorexia or other psychiatric disorders.
Conclusions
Despite recent increases in medical student numbers and the greater expectation that psychiatrists should be teaching undergraduates, there is little practical guidance available. However, specific educational sources and postgraduate training can improve a clinician’s basic teaching skills. Most clinical settings provide opportunities for teaching students, but these need to be tailored accordingly. Effective teaching has a number of benefits, not least that it may raise recruitment into psychiatry, which is still a shortage specialty. Current evidence tells us that we still have a long way to go to win the hearts and minds of prospective doctors for psychiatry, but providing a positive undergraduate experience for students may do much to alter this situation.
Declaration of interest
None.
MCQs
-
1 With regard to undergraduate teaching of psychiatry:
-
a the teaching commitments of consultants are likely to fall in the future
-
b students in foreign countries have a far more positive view of undergraduate psychiatry
-
c student experiences of teaching during a clinical placement have little bearing on future career choice
-
d our regulatory agencies do not regard teaching as a key professional skill required by all doctors
-
e teaching is described as supporting professional activity in the new consultant contract.
-
-
2 In relation to learning how to teach:
-
a most doctors have learned to teach through an apprenticeship model
-
b the acquisition of teaching skills may enhance a doctor’s value to an organisation or trust
-
c most psychiatrists have enough time to learn how to teach effectively
-
d distance-based teaching courses are appropriate for all clinicians
-
e much practical information on how to teach is freely available online.
-
-
3 With reference to student learning theory:
-
a a surface learning approach should be encouraged
-
b experiential learning dictates that the most effective learning occurs through a cycle of experience and reflection
-
c modelling of a teacher’s behaviour is likely to have negligible impact on a student’s learning and appreciation of psychiatry
-
d understanding your own learning and teaching style could help improve your students’ learning
-
e student learning is unlikely to be affected by day-today concerns such as suitable living accommodation and staff canteens.
-
-
4 Regarding teaching in different environments:
-
a most modern psychiatry undergraduate teaching occurs in medical school lecture theatres
-
b allocating a specific clinician to aid student teaching during clinical ward rounds is recommended
-
c hot-seating is a useful technique employed in clinic-based teaching
-
d asking students to follow up and provide regular reports on patients can be used as part of an effective teaching strategy
-
e care should be taken when teaching students in environments such as the patient’s home or a casualty department.
-
5 If problems occur in student placements:
-
a feedback to students should be prompt and positive wherever possible
-
b student pastoral issues are not the concern of a teaching consultant
-
c a student’s consistent lack of honesty should have little bearing in their placement feedback and their suitability to practice medicine
-
d if you believe that a student on placement with you has a mental illness you should treat it yourself
-
e your own punctuality may have an impact on a student’s time-keeping.
-
-
MCQ answers
| 1 | 2 | 3 | 4 | 5 | |||||
|---|---|---|---|---|---|---|---|---|---|
| a | F | a | T | a | F | a | F | a | T |
| b | F | b | T | b | T | b | T | b | F |
| c | F | c | F | c | F | c | T | c | F |
| d | F | d | F | d | T | d | T | d | F |
| e | T | e | T | e | F | e | T | e | T |





eLetters
No eLetters have been published for this article.