Introduction
Mental health is a core component of quality of life. Without it, people are likely to experience problems or distress in various aspects of their lives, including their relationships, their work and their physical health (Huppert and So, Reference Huppert and So2009; WHO, 2005). Improving mental health helps people to function more effectively at work and in society more generally (Dewe and Kompier, Reference Dewe and Kompier2008). People with higher levels of mental health achieve superior outcomes including better work performance, better social relationships and better physical health (e.g. Huppert, Reference Huppert2009; Lyubomirsky et al., Reference Lyubomirsky, King and Diener2005; Richman et al., Reference Richman, Kubzansky, Maselko, Kawachi, Choo and Bauer2005). Clearly mental health is an important resource that allows people to lead more successful and subjectively enjoyable lives.
Participating in work can significantly improve employee mental health and, importantly, facilitate effective recovery from mental illness. However, while being employed is better for mental health than being unemployed in general, it is important to note that jobs with poor psychosocial quality are worse for mental health than having no job at all (Butterworth et al., Reference Butterworth, Leach, Strazdins, Olesen, Rodgers and Broom2011). In this chapter, we explore the impact that work can have on mental health outcomes and what workplaces can do to enhance the wellbeing of those already employed. This includes looking at the ‘dark side’ of work and how workplaces can harm employee mental health, as well as what workplaces can do to enhance employee wellbeing. We argue that wellbeing-enhancing workplaces are those that both prevent the harmful aspects of work by identifying, assessing and managing stressful working conditions and enhance the health-promoting and-protective aspects of work.
Understanding Mental Health
It is well known that depression is predicted to be the main contributor to the burden of disease by 2030 (WHO, 2008). However, minimising depression does not, by itself, guarantee good mental health. Over the last two decades, researchers and mental health experts have significantly advanced their understanding of what it means to have good mental health. Increasingly, experts challenge a disease-based model of mental health, which defines mental health as the absence of mental disorder, and focus on a health-based model of mental health (Macik-Frey et al., Reference Macik-Frey, Quick, Quick, Nelson, Antoniou, Cooper, Chrousos, Spielberger and Eysenck2009). A health-based model defines mental health as a state of wellbeing or, more specifically, as the presence of positive emotional wellbeing (e.g. joy, happiness, contentment), psychological wellbeing (e.g. a sense of purpose, achievement and mastery) and effective social functioning (Diener, Reference Diener2000; Huppert, Reference Huppert, Huppert, Baylis and Keverne2005; Keyes, Reference Keyes2002, Reference Keyes2005; see also Chapter 8 of this volume).
The distinction between mental health as the absence of disease and mental health as the presence of wellbeing has broadened the array of models used to describe and measure mental health. Keyes’ (Reference Keyes2002, Reference Keyes2005) concept of good mental health or flourishing recognizes that optimal mental health includes both a low level of mental illness, including depression, and a high level of positive wellbeing. Only a small proportion of the population, at least in the United States, meets this criterion (17%), with the majority of people being only moderately mentally healthy (Keyes, Reference Keyes2005). Further, those with optimal mental health report fewer health limitations, missed work days and work cutback days and healthier psychosocial functioning than those with ‘incomplete’ mental health (i.e. not meeting the criteria for complete mental health), suggesting that mental health is best represented by considering mental health and mental ill health as separate but correlated constructs.
Understanding different approaches to defining and measuring mental health is important for informing the types of interventions that may be successful at enhancing wellbeing. Specifically, a more complete approach to mental health highlights the importance of both preventing the factors that harm mental health and promoting the factors that promote wellbeing or flourishing mental health.
Work and Mental Health
Work has real and demonstrable impacts on employee mental health outcomes. Both unemployment and underemployment are detrimental to mental health. However, while there are health benefits to being employed, being in poor-quality and stressful work is worse for mental health than having no job at all (Butterworth et al., Reference Butterworth, Leach, Strazdins, Olesen, Rodgers and Broom2011). Therefore, for those employed, work needs to be ‘good’ work if it is to be health-promoting (Black, Reference Black2008; Waddell and Burton, Reference Waddell and Burton2006). Importantly, working towards and accessing good work also plays a role in personal recovery from mental health problems, providing access to financial, psychological and social rewards, including a sense of self-worth, supportive relationships, goal attainment and achievement (see Chapter 3 of this volume).
Mental health problems are common amongst working people (Sanderson and Andrews, Reference Sanderson and Andrews2006). In 2007, the prevalence of lifetime-diagnosed depression in the Australian workforce was 12% amongst men and 18% amongst women (14.7% total) (LaMontagne et al., Reference LaMontagne, Sanderson and Cocker2010b). This is equivalent to 1.54 million people in the Australian population. Subclinical mental health problems and generalised distress, alongside clinical disorders such as major depression and generalised anxiety, are also prevalent in the working population (Hilton et al., Reference Hilton, Whiteford, Sheridan, Cleary, Chant and Wang2008; Sanderson and Andrews, Reference Sanderson and Andrews2006). Therefore, workplaces can play a role in supporting mental health promotion initiatives and the early identification of mental health problems amongst working people, thereby facilitating tertiary prevention efforts.
Work as a Determinant of Mental Health
The relationship between work and health is a matter of great importance to employees and employers alike. In industrialised countries, legislation covers many aspects of the conditions under which people work for pay, covering hours of work, health and safety, equal opportunity and employee and industrial relations. However, despite the presence of legislation, some work environments can be damaging to mental health (Butterworth et al., Reference Butterworth, Leach, Strazdins, Olesen, Rodgers and Broom2011). Poor-quality jobs are those where a person is exposed to psychosocially hazardous work conditions or job stressors. These are problems with the way work is designed or managed or in its social and organisational context (Leka et al., Reference Leka, Jain, Zwetsloot and Cox2010). Exposure to job stressors is widespread. In Australia, around 25% of working women and 18% of working men (roughly 1 in 4) experience job stress (LaMontagne et al., Reference LaMontagne, Keegel, Vallance, Ostry and Wolfe2008). Similar rates have been reported in Europe, where work-related stress affects one in three workers (European Agency for Health and Safety at Work, 2002).
Exposure to stressful working conditions, such as excessive job demands combined with little job control, predicts a range of negative employee outcomes, including psychological distress, depressive symptoms, depression, anxiety, suicide and other mental health problems (LaMontagne et al., Reference LaMontagne, Keegel, Louie and Ostry2010a; Michie and Williams, Reference Michie and Williams2003; Stansfeld and Candy, Reference Stansfeld and Candy2006). Other established psychosocial work factors known to predict mental health problems include a lack of social support at work, effort–reward imbalance and job insecurity (de Lange et al., Reference de Lange, Taris, Kompier, Houtman and Bongers2003; Rugulies et al., Reference Rugulies, Bultmann, Aust and Burr2006; Stansfeld and Candy, Reference Stansfeld and Candy2006).
Importantly, the presence of job demands alone does not necessarily indicate that people are engaged in ‘bad’ work. High job demands may benefit health when they are balanced by adequate organisational and personal resources. For example, active jobs which involve high demands in combination with high control or decision latitude can promote feelings of mastery (Karasek and Theorell, Reference Karasek and Theorell1990). Mastery is an important feature of psychological wellbeing (Ryan and Deci, Reference Ryan and Deci2000; Ryff, Reference Ryff1989). High job demands can also contribute positively to employee engagement – a positive, active state defined by the characteristics of vigour, absorption and dedication in pursuit of one’s work goals – when job resources, such as organisational climate, innovativeness and supervisor support are high (Bakker et al., Reference Bakker, Hakanen, Demerouti and Xanthopoulou2007).
There are many paths through which work can be beneficial to psychological well-being, contributing to feelings of self-esteem and self-worth and providing opportunities for employees to pursue goals, experience mastery and develop meaningful relationships (LaMontagne and Keegel, Reference LaMontagne, Keegel, Keleher and MacDougall2009; Waddell and Burton, Reference Waddell and Burton2006). The evidence base regarding what constitutes ‘good’ work, defined as having positive, health-promoting working conditions (Black, Reference Black2008), is underdeveloped relative to the evidence base regarding adverse or negative working conditions (LaMontagne et al., Reference LaMontagne, Martin, Page, Reavley, Noblet and Milner2014). However, research to date has identified a fair organisational climate and commitment to work, the ability of workers to exert control over the task they are doing (Holmgren et al., Reference Holmgren, Love, Mardby and Hensing2014), good communication in the workplace, high social support and manageable job demands at work as important elements of healthy work (Lowe et al., Reference Lowe, Schellenberg and Shannon2003). Some other potentially important elements include having meaningful work, being able to use one’s skills and strengths at work and experiencing growth and development through work (Black, Reference Black2008; Waddell and Burton, Reference Waddell and Burton2006). Positive and healthy leaders developing supportive and authentic leadership practices in the workplace, for example, are also an important conduit to healthy work (Macik-Frey et al., Reference Macik-Frey, Quick and Cooper2008; Quick et al., Reference Quick, Macik-Frey and Cooper2007; Quick and Quick, Reference Quick and Quick2004; Vella-Brodrick and Page, Reference Vella-Brodrick, Page and Sarros2009). Good work has been associated with a range of beneficial individual and organisational outcomes, including high work ability (Arnetz and Blomkvist, Reference Arnetz and Blomkvist2007; Lindberg et al., Reference Lindberg, Josephson, Alfredsson and Vingard2006) and self-rated health (Lohela et al., Reference Lohela, Bjorklund, Vingard, Hagberg and Jensen2009). The workplace is also an important setting for mental health promotion and early intervention regardless of cause (LaMontagne et al., Reference LaMontagne, Martin, Page, Reavley, Noblet and Milner2014).
Creating Wellbeing-Enhancing Workplaces
Given that work can have either a healthy or deleterious effect on mental health, wellbeing-enhancing workplaces are those that strive to prevent the factors that can harm mental health and promote the positive aspects of work and worker strengths and positive capabilities.
Preventing Harm: Managing and Preventing Stressful Working Conditions
Until recently, research on how to prevent stress was dominated by individual-level activities (LaMontagne et al., Reference LaMontagne, Keegel, Louie, Ostry and Landsbergis2007a): for example, teaching employees how to better manage stress through relaxation training or improving individual help-seeking behaviour for mental health problems. Although individually focused activities can positively impact a person’s stress response, and are therefore an important secondary prevention strategy, they have limited effectiveness over the longer term. Primary prevention strategies represent a more sustainable long-term approach to stress (LaMontagne et al., Reference LaMontagne, Keegel, Louie, Ostry and Landsbergis2007a). Primary strategies involve implementing organizational-level strategies that address stressors at their source, for example, targeting elements of the psychosocial working environment. The systems approach to job stress prevention involves the best of both primary- and secondary-level strategies. Primary preventative strategies typically occur at the organisational level and involve identifying and addressing stressors at their source (e.g. reducing workload or giving workers more control over their work). Secondary strategies are typically individually focused activities that help workers to respond more effectively to stressful working conditions, for example, teaching (LaMontagne et al., Reference LaMontagne, Keegel, Louie, Ostry and Landsbergis2007a, Reference LaMontagne, Keegel and Vallance2007b). A systems approach also requires active and meaningful employee participation and strategies that are tailored to an organisation’s specific context and needs (LaMontagne et al., Reference LaMontagne, Keegel, Louie, Ostry and Landsbergis2007a, Reference LaMontagne, Keegel and Vallance2007b).
However, while these systematic reviews indicate what to do, questions still remain regarding how to do it. Intervention strategies need to be tailored and context-appropriate (Biron et al., Reference Biron, Karanika-Murray, Cooper, Biron, Karanika-Murray and Cooper2012) to stand the best chance for success. This poses a problem in practice: the principles of preventing or managing stressful working conditions are necessarily broad, and considerable effort is needed to tailor solutions to unique work settings (e.g. accounting for how the business is run, worker sociodemographics and occupational skill levels, type of workplace, presence or absence of a union). Although knowledge of context-appropriate solutions for various work settings is growing, there is still a need to apply principles and develop solutions on an organisation-by-organisation basis. This has likely contributed to the slow uptake of effective job stress prevention and control strategies in practice; for example, Human Resources or OH&S staff commonly cite Employee Assistance Programs as their organisation’s response to job stress concerns (LaMontagne et al., Reference LaMontagne, Keegel and Vallance2007b). Other barriers to the implementation of evidence-based interventions stem from issues of stigma similar to those concerning mental illness in general, such as a persisting view of job stress as an individual weakness rather than an organisational issue (Page et al., Reference Page, LaMontagne, Louie, Ostry, Shaw and Shoveller2013).
Applying a systems approach to stress prevention would likely have a significant impact on both the prevalence and cost of work-related mental illness. LaMontagne et al. (Reference LaMontagne, Sanderson and Cocker2010b) found that, of the $12.6 billion annual costs accrued to society through major depression amongst working Australians, approximately $730 million was attributable to job strain. Further, the majority of these costs related to employment factors such as lost productivity, absenteeism, turnover and employee replacement costs. Importantly, evidence suggests that job stress – and the associated impacts on individual and organisational health – is preventable through improvements to the psychosocial working environment.
Promoting the Positive: Identifying and Developing the Positive Aspects of Work and Worker Capabilities and Strengths
There is also growing evidence regarding what workplaces can do to promote the positive aspects of work, including developing the positive aspects of work and worker strengths and capabilities. The relevant intervention principles and evidence in this area come predominantly from the fields of positive psychology, positive organisational behaviour and positive organisational scholarship (Macik-Frey et al., Reference Macik-Frey, Quick and Nelson2007; Macik-Frey et al., Reference Macik-Frey, Quick, Quick, Nelson, Antoniou, Cooper, Chrousos, Spielberger and Eysenck2009; Wright and Quick, Reference Wright and Quick2009). Positive psychology focuses on the conditions and processes that contribute to the flourishing or optimal functioning of people, groups and institutions (Gable and Haidt, Reference Gable and Haidt2005). Positively focused interventions apply strength-based methods to achieve positive outcomes. Strength-based methods are applied to identify and enhance strengths or what is being done well, rather than trying to identify and fix what is ‘wrong’ in an individual, group or organisation (Schaufeli, Reference Schaufeli2004). To date, research in this area has largely focused on individual-level interventions that enhance well-being (Gable and Haidt, Reference Gable and Haidt2005). However, there is considerable scope and appetite for more positive-psychology-based organisational-level wellbeing research. While there is not yet a preferred approach to promoting the positive aspects of work, initial research suggests that important gains can be made when organisations invest in the development of positive leaders, provide access to meaningful work and promote a positive organisational climate (Cameron, Reference Cameron2008; Cameron et al., Reference Cameron, Dutton and Quinn2003; Cotton and Hart, Reference Cotton and Hart2003; Macik-Frey et al., Reference Macik-Frey, Quick and Cooper2008; Quick et al., Reference Quick, Macik-Frey and Cooper2007; Quick and Quick, Reference Quick and Quick2004).
Wellbeing-Enhancing Workplaces in Practice
Recognising that both individual and workplace factors play a role in preventing stress and promoting wellbeing, workplaces need to implement activities at multiple levels within the organisation to be most effective at promoting employee wellbeing. Wellbeing activities also need to integrate wellbeing promotion and stress prevention. This ensures that strategies cover both sides of the illness-to-wellness continuum. Last, to be both sustainable and effective over the longer term, workplaces need to take a strategic approach to managing wellbeing and mental health in the workplace. But what does this look like in practice?
Our team has devoted the majority of our careers to investigating what works to prevent stress and promote wellbeing in the workplace from a practical perspective. Like many practitioners in this space, my (first author) intervention efforts started at the individual level. My doctoral studies involved designing and testing a positive-psychology-based employee wellbeing program. The program, called the Working for Wellness Program, consisted of six one-hour sessions delivered to full-time employees in small groups (Page and Vella-Brodrick, Reference Page and Vella-Brodrick2010). The sessions covered a number of empirically supported positive psychology strategies including knowing and using strengths, striving for self-concordant goals, getting into flow and cultivating positive relationships. Program participants reported significant increases in wellbeing following the program in comparison to a randomly selected control group (Page and Vella-Brodrick, Reference Page and Vella-Brodrick2010). From here, I designed and tested a number of other employee wellbeing programs, including a team-based version of the Working for Wellness Program, and later collaborated with a mental health foundation (SuperFriend.com.au) to develop a positive-psychology-based online wellbeing program for teams (http://www.teamtopia.com).
Later, our team was funded by the Victorian Health Promotion (VicHealth) to design a leadership-based stress prevention program, called Creating Healthy Workplaces. Most recently, we expanded the Creating Healthy Workplaces program to include a mental health promotion element in collaboration as part of a broader research team. The latter program, funded by VicHealth and the Victorian WorkCover Authority, is currently being evaluated by a cluster randomised control design, funded by a National Health and Medical Research Council Partnership grant. Our collective experience in this area has enabled us to collect a number of evidence-based but practical insights into what workplaces can do to prevent stress and enhance wellbeing. We have found that most workplaces commence their well-being journey through the provision of various nonintegrated and ad hoc wellbeing or mental health initiatives and then, over time, move towards more sophisticated and integrated initiatives (see Figure 23.1 for a diagrammatic representation of this). Most commonly, nonintegrated or ad hoc workplace wellbeing strategies include Employee Assistance Programs and lunchtime wellbeing seminars. Ad hoc initiatives are rarely effective and are often viewed by employees as a ‘nice to have’ or optional extra. Over time, some employers move towards more sophisticated efforts. Such efforts are often championed by a single passionate individual or motivated by a significant workplace event (e.g. a high-profile health and safety event), both of which can help to create organisational readiness to change.
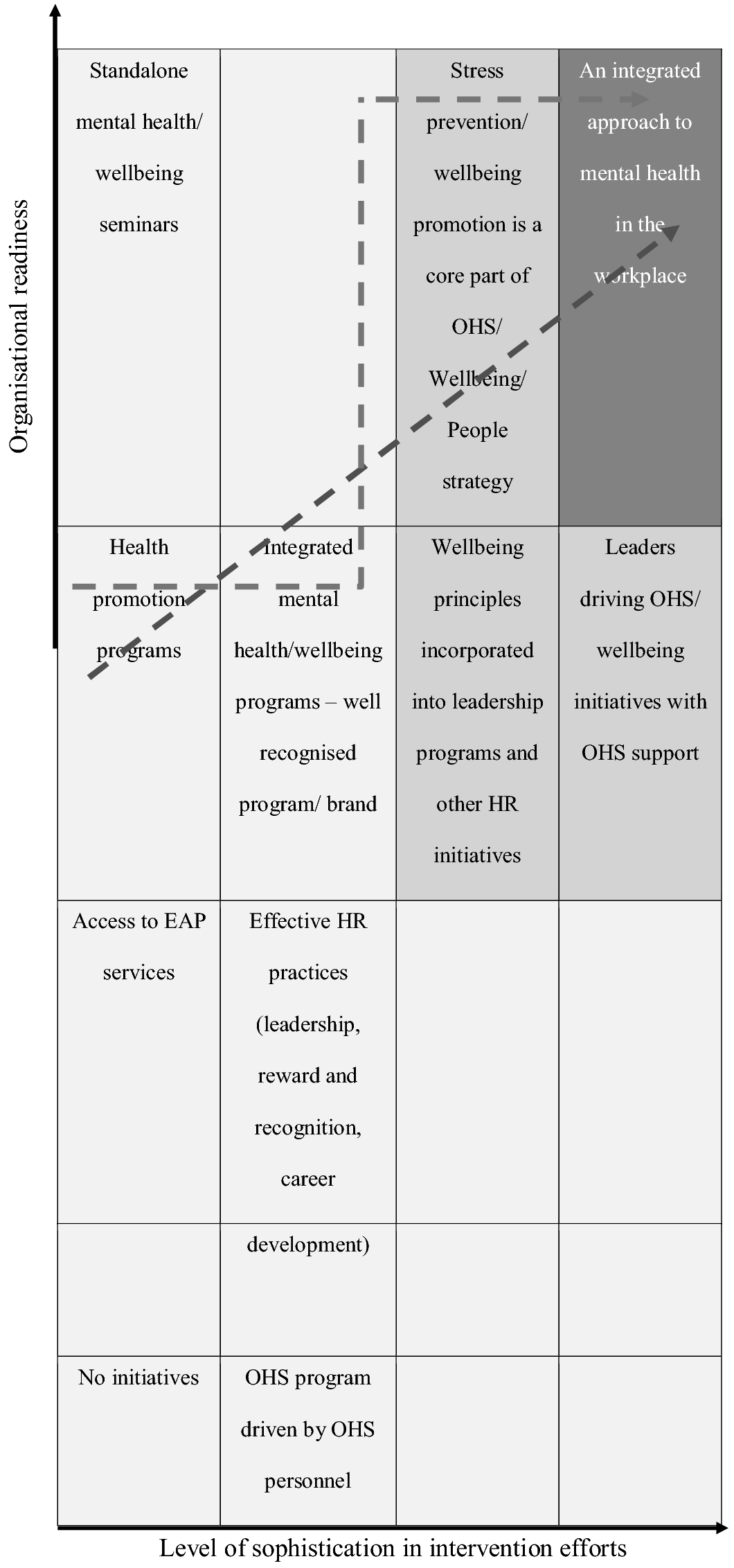
Figure 23.1 Pathways towards an integrated approach to workplace mental health.
Although, as Figure 23.1 shows, there are multiple possible pathways towards workplace mental health, there are things workplaces can do to improve their chances of building a wellbeing-enhancing workplace.
Table 23.1 summarises a number of enablers for creating wellbeing-enhancing workplaces, which we identified in a recent SuperFriend study (Page et al., Reference Page, Milner, Tchernitskaia and LaMontagne2014). As described here, some of the most successful efforts we have seen are those where wellbeing is integrated into the human capital or people strategy. This ensures that wellbeing is of strategic importance within the organisation and prioritised accordingly. Organisations that make leaders and managers accountable for driving wellbeing initiatives also tend to be more effective. This sends a strong message to the workplace that staff wellbeing is important. Like any business initiative, it is important that wellbeing initiatives are implemented according to sound business and organisational change principles. This includes setting real and measurable targets, tracking progress and coupling projects with well-thought-out communication and change action plans. Another useful idea is to incorporate wellbeing messages and strategies into existing programs, including leadership development and induction programs. This helps to ensure that wellbeing is integrated right across the employee lifecycle rather than being a standalone initiative. We also believe wholeheartedly in the importance of innovation and creative thinking to ensure that wellbeing initiatives are ‘front and centre’ in people’s minds. Organisations must continually refresh wellbeing initiatives if they are to become embedded in the organisation’s culture.
| Success factors | |
|---|---|
| • Be strategic: Wellbeing and mental health needs should be a fundamental factor within the company’s workforce (e.g. human capital) strategy (alongside or within safety). | • Build credibility with the executive team by demonstrating an understanding of business risks and needs and delivering on objectives. |
| • Make leaders and managers accountable for driving initiatives, with the support of OH&S and HR. Promote this level of commitment to the broader organisation, for example by displaying leadership commitment statements, signed and dated by a member of the executive team. | • Learn from others who have applied strategies in other organisations; incorporate case stories from other well-respected organisations in your business cases. |
| • Deliver strategies according to sound business and organisational change principles. This includes effective long-range planning – potentially planning for less but executing well in order to deliver on KPIs and achieve the desired outcomes. | • Integrate workplace mental health messages into existing HR or OH&S initiatives or programs, for example leadership training. Leverage from what has worked in the past. |
| • Draw on effective marketing and communication principles (and internal resources, where possible) to get clear, consistent messages across and engage all levels of an organisation. | • Innovate. Organise major events that increase the visibility of safety/wellbeing. Use word of mouth well. Refresh and reinvigorate efforts regularly. Ensure systems support rather than thwart innovation. |
| • Upskill HR or OH&S professionals regarding how to integrate optimal mental health strategies into a workforce strategy. | • Recruit/support/leverage from passionate OHS managers/senior-level staff members. |
Note: Refer to superfriend.com.au for more information.
Summary and Conclusion
The benefit of work to mental health and recovery from mental ill health has been well noted. However, while in general, employment is better for mental health than being unemployed, it is important to note that jobs of poor psychosocial quality are worse for mental health than having no job at all (Butterworth et al., Reference Butterworth, Leach, Strazdins, Olesen, Rodgers and Broom2011). In this chapter, we explored the impact that work can have on mental health outcomes and what workplaces can do to enhance the wellbeing of those already employed. First, we outlined the importance of identifying, assessing and managing stressful working conditions in order to prevent harm to worker mental health. Next, we considered how workplaces can promote the positive aspects of work, including employee strengths and positive capabilities. Finally, we highlighted several potential pathways through which workplaces can prevent job stress and promote employee wellbeing.
A key point in this chapter is that there is no one right way to create a wellbeing-enhancing workplace. Workplaces can build momentum towards more enduring and sustainable workplace programs, such as those discussed here, by starting with smaller initiatives. It is critical that senior managers understand why wellbeing is important in order to invest in these larger programs, and sometimes this becomes evident through frequent, smaller initiatives. However, although these smaller efforts are useful in the shorter term, workplaces must work towards more sophisticated efforts. This should involve regularly assessing the psychosocial work environment for risks to mental health, implementing tailored stress prevention and wellbeing promotion programs at both the organisational and individual level, evaluating the success of these efforts and ensuring that workers are meaningfully engaged in the process. Although these initial investments may seem onerous, the value of promoting wellbeing, for individuals, business and society, has been well documented, and wellbeing promotion can have a lasting impact over time.