Introduction
Psychoactive drugs, whether illicit or prescribed, are commonly used by people either recreationally, to self-medicate physical or psychological distress, or as part of social or cultural rituals. Many people use them with no concerns, but a significant proportion develop physical, psychological or social problems that will come to the attention of their doctor. These problems occur across a spectrum, with drug dependence at one end. Dependence involves the concepts of tolerance (needing increasing amounts to achieve the same effects) and withdrawal symptoms, but also loss of control of drug use such that use continues despite obvious adverse consequences. Drug use is heavily influenced by the individual’s social environment, and is usually initiated and maintained through contact with others.
The general practitioner (GP) should be aware of the possibility that drug use is causing or influencing presenting problems, and be able to make an appropriate assessment, provide advice and information and signpost other help where required.
Who Uses Drugs and Why?
How Likely Is a GP to See Someone Who Uses Drugs?
The main sources of information about the prevalence of illicit drug use in adults in the United Kingdom are household surveys such as the Crime Survey for England and Wales (CSEW), which has run since 2001/02 (United Kingdom Focal Point on Drugs, 2014). Such surveys consistently report that cannabis is the most commonly used illicit drug (see Table 17.1). Cocaine is the second most commonly used, followed by ecstasy (methylenedioxymethamphetamine [MDMA]). The highest rates of illicit drug use are reported by young adults, and the risk for initiation into illicit drug use decreases after the age of 20. Surveys specifically of young people also show that cannabis is the most prevalent drug used, with 16–19 per cent of 15-year-old respondents in England and Scotland reporting having used cannabis (UK Focal Point on Drugs, 2014).
Table 17.1 Percentage of 16–59-year-olds reporting lifetime and last-year use of individual drugs by sex in England and Wales 2013/14
| Lifetime use | Last-year use | |||||
|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | |
| Any drug | 41.1 | 30.3 | 35.6 | 11.8 | 5.8 | 8.8 |
| Amphetamines | 14.0 | 8.3 | 11.1 | 1.1 | 0.5 | 0.8 |
| Cannabis | 35.1 | 24.9 | 29.9 | 9.1 | 4.1 | 6.6 |
| Cocaine (incl. crack) | 12.1 | 6.9 | 9.5 | 3.4 | 1.4 | 2.4 |
| Ecstasy | 12.1 | 6.4 | 9.3 | 2.3 | 0.9 | 1.6 |
| LSD | 7.5 | 3.1 | 5.3 | 0.5 | 0.1 | 0.3 |
| Magic mushrooms | 10.1 | 4.6 | 7.3 | 0.6 | 0.1 | 0.4 |
| Opioids | 1.6 | 0.6 | 1.1 | 0.3 | 0.1 | 0.2 |
(UK Focal Point on Drugs, 2016, at www.gov.uk/government/uploads/system/uploads/attachment_data/file/669021/UK-drug-situation-2016-report.pdf . Accessed 22 January 2018.)
Overall, drug use in the United Kingdom has declined over the past 10 years, but it would be wrong to assume that this means that the problem of illicit drugs is disappearing. When considered generation by generation since World War II, rates of illicit substance use have increased across each successive five-year cohort in developed countries (Degenhardt et al., Reference Degenhardt, Lynskey and Hall2000). The age of initiation into both licit and illicit drugs has declined over this period, and this is important because an earlier age of onset for substance use is associated with higher levels of dependence, and swifter and more severe problem development. In recent cohorts there is greatly increased exposure to illicit drugs and the opportunities to use them, meaning that use of illicit substances has become increasingly normalized (Darke, Reference Darke2011).
Problem drug use is defined in different ways in different countries, for example, in England estimates are available of the number of opioid and/or crack cocaine users and injecting drug users. Latest estimates for the United Kingdom (2004–2011) suggest that there were 330,455 high-risk opioid users, which corresponds to a rate of 8.1 per 1,000 inhabitants aged 15–64. There were an estimated 122,894 injecting drugs users, or 3.0 per 1,000 inhabitants aged 15–64 (EMCDDA Statistical Bulletin, 2016 www.emcdda.europa.eu/data/stats2016).
Risk Factors for Drug Use and Related Harm
Different risk factors have been shown to be important at different life stages, and risk factors that accumulate across the course of development can additively impact substance use and related harms (Loxley et al., Reference Loxley, Toumbourou and Stockwell2004). Furthermore, there is evidence for a cascading effect of risk factors with time, for example, exposure to maternal drug and alcohol use can cause developmental delays that increase exposure to subsequent risk factors such as poor school adjustment. However, a number of protective factors have also been identified.
Pre-Birth: Being born or raised in a family experiencing extreme economic deprivation is a risk factor for harm associated with drug use, and being born or raised in a sole-parent household is a risk factor for more frequent drug use in adolescence.
Pre- and Primary School Period (0–11): Child neglect and abuse is a risk factor for impaired child development, leading to a pathway of poor child adjustment and so harmful drug use. However, an easy, shy or cautious temperament in early childhood may act as a protective factor for positive child adjustment and reduce the influence of other risk factors, leading to lower rates of involvement in harmful drug use.
Secondary School (12–17): Risk factors for harmful drug use in this period relate to
the community (low involvement in activities with adults, perceived and actual levels of community drug use, a positive media portrayal of drug use and community disadvantage and disorganization)
parents (parent–adolescent conflict, favourable or permissive parental attitudes to drug use or parental alcohol or drug problems)
peers (peer drug use)
the individual (sensation-seeking and adventurous personality, favourable attitudes to drug use)
Protective factors include religious involvement, family attachment, low parental conflict and parent–adolescent communication.
How Can the GP Identify Potential Drug Issues?
Diagnosis
The diagnostic terminology can seem muddled, and has been subject to change over time. The usual approach is to consider substance use across a spectrum:
Use – regular use – ‘risky’ use – problematic use – dependence
The dependence syndrome refers to what most people think of as ‘addiction’. It refers to ‘a cluster of physiological, behavioural, and cognitive phenomena in which the use of a substance takes on a much higher priority for a given individual than other behaviours that once had greater value’ (World Health Organization, 1992). A key feature is a strong and often overpowering desire to take psychoactive drugs, and a sense of loss of control over when to use and in what quantity. The individual often feels powerless to overcome a desire to use, even faced with evidence of the problems the drug is causing them. The latest version of the North American Diagnostic and Statistical Manual (DSM-5) has abandoned the distinction between abuse and dependence, replacing them with a single category of Substance Use Disorder, which in turn may be mild, moderate or severe. However, the concept of dependence is still useful in guiding treatment, as once it has developed the best course of action is likely to be abstinence from the problem substance.
What Harms Do Illicit Drugs Cause?
A number of authors, notably David Nutt and colleagues (Nutt et al., Reference Nutt, King and Phillips2010), have considered the problems associated with drug use by examining the physical harms, dependence potential and social harms associated with different substances (including alcohol). The modelling concluded that heroin, crack cocaine and methamphetamine (‘crystal meth’) were the most harmful drugs to individuals, whereas alcohol, heroin and crack cocaine were the most harmful to others. Overall, alcohol was the most harmful substance followed by heroin and crack cocaine.
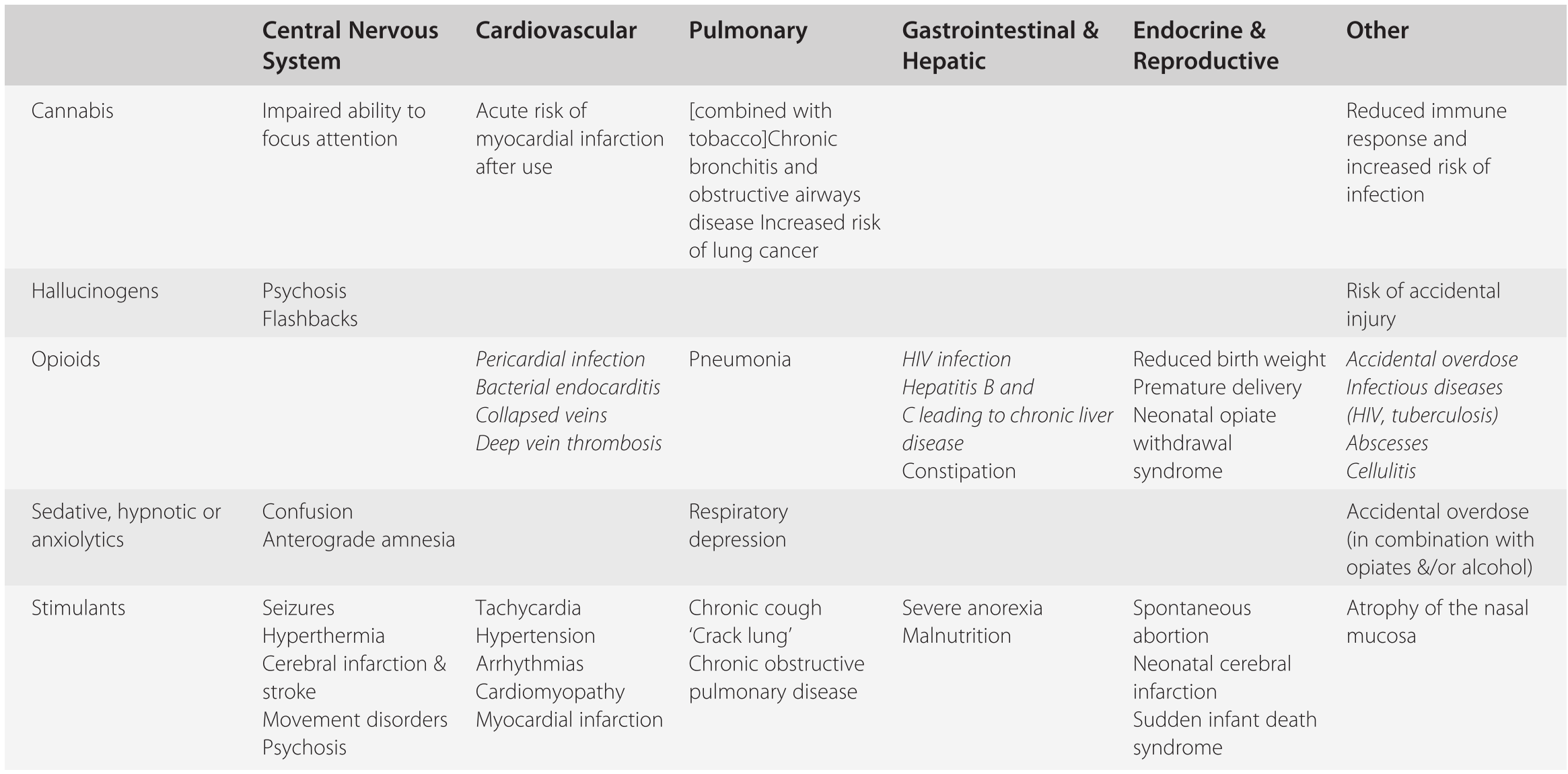
Physical Consequences
Drug use carries a wide range of possible physical consequences, often specific to the drug or the route through which it is administered. At one end of the spectrum, drug use may lead directly to death from overdose (the risk of which is generally higher when drugs are injected). Drug use can also lead to harm indirectly by precipitating specific medical conditions, for example, cirrhosis, seizures, strokes, cardiomyopathy and peptic ulcers. Drug use may additionally shorten life due to its contribution to the risk of road traffic accidents, lung cancer, suicide or blood-borne virus (e.g. HIV) transmission, or a variety of other acute and chronic conditions (Day & Khurmi, Reference Day, Khurmi, Gray and Cormac2012) (see Table 17.2).
| Central Nervous System | Cardiovascular | Pulmonary | Gastrointestinal & Hepatic | Endocrine & Reproductive | Other | |
|---|---|---|---|---|---|---|
| Cannabis | Impaired ability to focus attention | Acute risk of myocardial infarction after use | [combined with tobacco] Chronic bronchitis and obstructive airways disease Increased risk of lung cancer | Reduced immune response and increased risk of infection | ||
| Hallucinogens | Psychosis | Risk of accidental injury | ||||
| Flashbacks | ||||||
| Opioids | Pericardial infection | Pneumonia | HIV infection | Reduced birth weight | Accidental overdose | |
| Bacterial endocarditis | Hepatitis B and C leading to chronic liver disease | Premature delivery | Infectious diseases (HIV, tuberculosis) | |||
| Collapsed veins | Constipation | Neonatal opiate withdrawal syndrome | Abscesses | |||
| Deep vein thrombosis | Cellulitis | |||||
| Sedative, hypnotic or anxiolytics | Confusion | Respiratory depression | Accidental overdose (in combination with opiates &/or alcohol) | |||
| Anterograde amnesia | ||||||
| Stimulants | Seizures | Tachycardia | Chronic cough | Severe anorexia | Spontaneous abortion | Atrophy of the nasal mucosa |
| Hyperthermia | Hypertension | ‘Crack lung’ | Malnutrition | Neonatal cerebral infarction | ||
| Cerebral infarction & stroke | Arrhythmias | Chronic obstructive pulmonary disease | Sudden infant death syndrome | |||
| Movement disorders | Cardiomyopathy | |||||
| Psychosis | Myocardial infarction |
Items in italics occur when drug is used intravenously
Psychological and Social Consequences
Mood disorders secondary to drug use and the associated lifestyle are common, and often manifest as mild-to-moderate anxiety or depression. Some people have more severe mood disorders, and these may be exacerbated by or caused by their drug use. In other cases there may be an attempt to self-medicate underlying mental health symptoms with drug use. Some drugs, most notably cannabis and stimulants, are associated with an increased risk of psychosis. This may be dose-related and short-lived, but the drug may also precipitate a prolonged episode of illness (Moore et al., Reference Moore, Zammit and Lingford-Hughes2007).
Drug dependence is associated with guilt, stigma and social isolation, and illicit users can be driven to poverty, criminality and imprisonment, damaging relationships with family and friends and limiting employment opportunities in the process. Society as a whole is also harmed by drug use, with significant economic costs arising from increased use of health care, policing, prisons, social services, insurance and loss of productivity.
Presentation and Treatment Options
Drug users may present in primary care in a number of different scenarios:
As a direct request for help
With the consequences of their drug use
Physical – for example, abscesses or infections, or after an overdose
Psychological – for example, with symptoms of anxiety or mood disorder
Social – for example, the involvement of social services with respect to childcare issues
Via a concerned family member
People with drug dependence, particularly injecting drug users, have higher rates of poor health, as well as a significantly increased risk of mortality. They are often frequent attenders of health services, and all GPs should be able to recognize the possibility of drug use in such scenarios and be able to take an adequate history to assess this.
Exploring the possibility of problematic drug use by asking simple questions such as ‘Do you use any illicit drugs?’ is an important first step, possibly followed up by asking about use of prescribed medication for reasons other than initially intended. Once established, it is important to ascertain the complexity of the problem by establishing the level of drug use and the problems that it may be causing:
Which drugs? (including alcohol, prescribed drugs, benzodiazepines)
How much and how often? (asking about daily monetary spending is an easy way of gauging how much is used)
Which route? (injecting, snorting, smoking, swallowing)
How long have they been using? (Have there been previous treatment episodes?)
This should be underpinned by advice that aims to reduce the risks that an individual is exposing themselves to by modifying their drug-taking behaviour. National guidance is clear that all community health practitioners should be able to deliver relevant harm reduction advice to drug users (Department of Health [England] and the Devolved Administrations, 2007). This should include:
Basic advice
Avoid injecting where possible (overdose risk is reduced by smoking)
If you do inject, reduce the risk by not mixing drugs, not using alone or reducing the amount used after periods when tolerance is reduced.
Action to prevent blood-borne virus transmission
Not sharing injecting paraphernalia, access to needle exchange, safe sex advice
Referral to specialist agencies where appropriate
Jo is a 28-year-old woman who has recently registered with the practice after having moved to the area. She attends an appointment with the GP and states that she ‘needs help with my drug use’.
She reports use of heroin and crack cocaine for five years, not currently injecting (but has done so in the past); she has recently moved in with her sister with the intention of addressing her drug use.
She admits to taking occasional illicit diazepam, but denies other drug use and only very occasionally drinks alcohol. She has been detoxified in prison (three years ago), and had contact with the local drug treatment service in the area she has just moved from, but she has never consistently engaged in treatment.
She has a history of mild depression, but is not on any treatment at this time. She has a pending court case for shoplifting, and admits that this is one of the triggers that has led her to seek help.
She does not have children, and there are no children at her sister’s house.
This initial consultation is an important first step to engage Jo into drug treatment. By being empathic and non-judgemental, by listening and by explaining the rationale for management decisions, the GP should be able to start to build a rapport and promote treatment retention.
The next steps will be dictated by the management options open to the GP: whether Jo can be treated in primary care or needs to be referred to specialist services. The GP can also use the opportunity to consider Jo’s physical and mental health. An initial consultation such as this can be time-consuming in a standard GP surgery, and it would be useful to bring Jo back for further booked appointments to address all of the relevant areas.
Drug users will often report negative experiences of contact with health services, including a feeling that they are not listened to, or that barriers were put up to accessing relevant support. In addition to the aforementioned basic exploration of patients’ drug use, GPs play an important role in performing general health checks, screening for hepatitis B, hepatitis C and HIV, ensuring that drug users are vaccinated appropriately, offering sexual health and contraception advice, and signposting to partner agencies for provision of needle exchange, psychological interventions, support with housing and benefits and specialist prescribing treatment.
Many people will take more than one substance, both together and separately, and this can lead to cumulative risks. In some cases, there is a primary problem substance, which if stopped will lead to cessation of use of the other substance. In others, the problematic use of more than one substance needs to be addressed concurrently.
Heroin and Opioids
Opioids such as heroin are taken because they lead to feelings of well-being, relaxation and euphoria. Regular users soon develop tolerance to opioids, leading to an increased frequency and quantity of use and physical dependence, with a significant withdrawal syndrome if they cease using abruptly. It is estimated that one in four people who try heroin go on to develop dependence, the second highest rate of dependence liability after tobacco (Regier et al., Reference Regier, Farmer and Rae1990). Females and males are equally likely to become heroin dependent, although subsequent higher rates of prevalence in males reflect differences in opportunity and uptake. Dependence on opioids is particularly debilitating and frequently associated with multiple social and psychological sequelae (Darke, Reference Darke2011).
Heroin is usually taken by smoking or injecting, and can lead to overdose and death via respiratory depression. This risk is increased if the drug is injected, particularly with concurrent use of other sedating drugs such as benzodiazepines or alcohol. Sharing injecting paraphernalia puts users at risks of transmitting blood-borne viruses, and long-term use of opioids is associated with chronic constipation, poor dentition and premature death.
Heroin users are usually dependent when they present to treatment, and treatment takes the form of opioid substitution treatment (OST) in conjunction with psychosocial interventions. The rationale of OST is to replace inconsistent, erratic and high-risk use of heroin with a longer-acting opioid taken at a stable dose with the intention of significant reduction or cessation of heroin use. The two most commonly used forms of OST are methadone and buprenorphine (Connock et al., Reference Connock, Juarez-Garcia and Jowett2006).
Methadone has been used in OST since the 1960s, and is prescribed as a 1 mg/ml oral solution. It is a full opiate agonist with a long half-life, and it can therefore take a few weeks to safely titrate the dose to therapeutic levels. This does not tend to cause significant issues, and evidence suggests that higher-level users of heroin settle best with flexible methadone regimes.
Buprenorphine is prescribed as a sublingual tablet and is a partial opiate agonist, meaning that high doses produce less euphoria, sedation and respiratory depression than methadone. Doses can be titrated to therapeutic levels rapidly (over a few days), and the pharmacology of the drug means that there is a risk of causing ‘precipitated withdrawal’ if it is taken too soon after other opioids are taken, and it ‘blocks’ the effect of other opioids during treatment if the dose is sufficiently high.
There is a developing evidence base for the provision of intramuscular naloxone to injecting or high-risk opioid users with the goal of prevention of accidental overdose (Strang & McDonald, Reference Strang and McDonald2016). Most overdoses are witnessed, and opiate users have shown themselves to be willing and able to intervene to save the life of friends or acquaintances. The United Kingdom has altered enacted legislation to allow naloxone to be used without a prescription in specific emergency circumstances, in a similar way to the use of adrenaline in anaphylaxis.
Concurrent psychosocial interventions (PSI) are a crucial component of treatment, and the evidence base demonstrates that treatment outcomes are significantly improved when OST is prescribed in conjunction with the delivery of PSI. Because of this, GPs should not prescribe OST in isolation, and ideally such prescribing should only take place in a ‘shared care’ environment where drug workers deliver PSI alongside the input of the GP. Psychosocial interventions are usually structured around a care plan which is regularly reviewed and backed up by an assessment of risk.
Stimulants
Psychostimulant drugs come in powder form which can be injected, snorted or swallowed, for example, cocaine or amphetamine, or in a smokeable freebase form, for example, crack cocaine. These drugs make the user feel more alert, confident and sociable, but can also lead to disinhibited behaviour. After effects may include fatigue, depression, paranoia and depersonalization. The beneficial mental effects of use and the depressant nature of withdrawal tend to promote binges. Many users of stimulants use them in a non-problematic fashion and do not present for treatment, but may present in primary care with other symptoms such as mood disorders or anxiety. Other users develop a more problematic pattern of use, and benefit from formal psychosocial interventions and advice to assist in modification or cessation of their drug use. There is no evidence base for prescribing replacement stimulants or other medications on a long-term basis for stimulant users in primary care.
Methylenedioxymethamphetamine (MDMA, ‘Ecstasy’)
Ecstasy has both stimulant and hallucinogenic properties. It enhances sensory perceptions and can produce states of altered consciousness and visual illusions, in combination with tachycardia, dry mouth, dilated pupils and facial muscle stiffness. Tiredness, muscle aching and headache may be present 24 hours after taking the drug. Deaths have been reported in occasional users of ecstasy, often after taking only one tablet. Such deaths are rare and the cause is variable, but hyperthermia is a characteristic feature.
Cannabis
Cannabis is the most commonly used illicit substance in the United Kingdom, and is predominantly taken by users for its relaxant and euphoric effects. Many use it in a non-problematic way, but a significant proportion (about 10 per cent) develops dependence. New techniques for growing cannabis mean that strains with a higher concentration of the main psychoactive ingredient, tetrahydrocannabinol (THC), are more prevalent, and this may have implications for the potential harms that can be caused.
Smoking cannabis probably increases cardiovascular disease risk in middle-aged adults, and as most joints of cannabis are rolled with tobacco there are implications for respiratory function and risk of cancer. Evidence is emerging that driving while cannabis-impaired approximately doubles the risk of having a crash. As described earlier, cannabis use is usually initiated between the ages of 15 and 25, an important period of brain development. Regular cannabis use in adolescence approximately doubles the risks of leaving school early and of cognitive impairment and psychoses in adulthood. It is also associated strongly with the use of other illicit drugs. These associations persist even when plausible confounding variables are controlled for in longitudinal studies. This suggests that cannabis use is a contributory cause of these outcomes, but it is also possible that these relationships are explained by shared causes or risk factors (Hall, Reference Hall2015).
The mainstay of treatment for problematic cannabis use is psychosocial interventions, though many cannabis users are also dependent on tobacco and a concurrent approach at smoking cessation may be beneficial. Dependent cannabis users may present with depressive symptoms in primary care, and it is usually recommended to defer both diagnosis of depression and consideration of antidepressant use for at least two to four weeks after cessation of cannabis use when withdrawal symptoms have abated.
Novel Psychoactive Substances
Novel psychoactive substances (NPS) – previously known as ‘legal highs’ – describe a disparate group of substances including stimulants, hallucinogens, sedatives and synthetic cannabinoids. The recent Psychoactive Substances Bill (2016) has legislated that all new psychoactive substances are illegal, replacing the previous system where new substances were frequently created to enable their legal sale, often as chemical modifications of similar substances.
Because of the multiple different effects and potential harms, it is important to identify with the patient which substance(s) they are taking, and advise management accordingly. The recent NEPTUNE project provides a useful sourcebook for understanding the potential harms of novel psychoactive substances and highlights possible management strategies (Abdulrahim et al., Reference Abdulrahim and Bowden-Jones2015).
Benzodiazepines
Benzodiazepines are widely used in clinical practice as anxiolytics and hypnotics but are associated with significant problems when taken long term, including over-sedation (which can lead to falls and fractures), forgetfulness, emotional blunting and low mood. Such effects are more pronounced in the elderly and at higher doses. Tolerance and withdrawal occur after prolonged use, leading to anxiety, panic attacks, suicidal thoughts, insomnia and potentially seizures. Clinical guidelines have long stated that they should be prescribed for a maximum of two to four weeks (National Collaborating Centre for Mental Health, 2011), but in practice, many people take them for much longer. It is estimated that up to 1 million people in the United Kingdom are dependent on benzodiazepines (Ashton, Reference Ashton, Haddad, Dursun and Deakin2004). Successful withdrawal is possible in most dependent patients, but consideration needs to be given to when and how to detoxify as extra help and services may be needed.
Benzodiazepine misuse is a serious problem in people who use illicit drugs (Gossop et al., Reference Gossop, Marsden and Stewart2003), but little evidence is available to guide practitioners in management. If there is concurrent opioid dependence, this should be treated first (with opioid substitute treatment). Many patients are then able to control their benzodiazepine use without the need for prescribing. If use of benzodiazepines persists and the patient is dependent, a structured detoxification may be appropriate. In such cases, an assessment should be made as to whether the user is dependent on benzodiazepines. This should come from history and symptoms, supported by at least two consecutive positive urine screens with no negative screens in the preceding four months. If the user is dependent, then prescribing is a treatment option, although the benefits should outweigh the risks (including diversion to others). Prescribing is not an option for non-dependent or binge users, for whom psychological interventions are the mainstay of treatment.
The goal of benzodiazepine prescribing is cessation of illicit benzodiazepine use, with a longer-term goal of a structured reduction and detoxification. There is no evidence to support the use of maintenance prescribing, and this may increase the associated risks. Before starting such a reduction, prescribers should ensure any underlying physical or psychiatric health problems are addressed, and educate the patient about the problems of long-term use, process of withdrawal and possible effects.
Conversion of the benzodiazepine of abuse to an equivalent dose of diazepam is the best strategy. The long half-life of diazepam allows a smooth and gradual withdrawal, and the different tablet strengths available allow flexibility when planning dose reductions. Diazepam can be issued on an FP10(MDA) interval prescription, allowing for daily collection from the pharmacy and thus protecting against overuse. It is rarely appropriate to start a dose of more than 30 mg diazepam daily (a dose which will prevent withdrawal fits) and often a lower starting dose may be appropriate. Longer-term prescribing must always be balanced against the risks, especially the negative effects on memory and cognitive skills, and should not be standard practice. Prescribing should cease if illicit benzodiazepine use persists, or if there is concurrent alcohol dependence. Comprehensive guidance is available for both prescriber and patient (Ashton, Reference Ashton2005).
Addiction and Pain Management
It has increasingly become an expectation of patients that modern medication will allow them to be pain free. Evidence suggests that an increase in prescription of opioids for pain is accompanied by an increase in prescription drug misuse and increased risk of morbidity and mortality (Stannard, Reference Stannard2012). Although research literature has shown some efficacy of opioids in chronic non-cancer pain, it is unclear how long this lasts, and strong opioids are not equally effective for all patients or for all types of pain. Pain and addictive disorders should be placed on a continuum rather than being seen as mutually exclusive.
The Danger of Creating Addiction
The goal of pain treatment is to decrease pain and improve function while monitoring for any adverse side effects. The therapeutic regimen must ‘do more for the patient than to the patient’, and should improve, not worsen, their quality of life. However, it is rarely easy to identify the small group of people who are at risk of developing opioid addiction as a diagnosis of dependence is made prospectively over time. Furthermore, having an addictive disorder does not rule out a treatable chronic pain problem.
A useful guide developed by Gourlay and colleagues suggests adopting ‘universal precautions’ in pain medicine, the cornerstone of which is the trial of opioid therapy with a clear plan to terminate the trial if opioids are ineffective (Gourlay et al., Reference Gourlay, Heit and Almahrezi2005). This methodology has a number of components, including identifying and addressing treatable causes of pain, undertaking psychological assessment (including the risks of addictive disorders), clearly stating the plan and gaining the patient’s consent that the use of opioids is a therapeutic trial, and ongoing assessment of pain level, function and co-morbid conditions, including possible addiction. Review should assess the ‘4 As’ of pain medicine – analgesia, activity, adverse effects and aberrant behaviour. Such an approach from the outset of the use of opioid analgesia will prevent the common primary care scenario of increasingly high doses of prescribed opioids that are ineffective, resulting in a patient still in pain but now also addicted to opioids. GPs should be confident with a management plan to cease the use of opioids after a defined short period of time if they are not effective, rather than increasing the dose.
Patients who develop dependence on opioids, either prescribed or over-the-counter, can be safely and effectively managed by their GP, although sometimes it is necessary to seek advice from specialist substance misuse treatment services. Such patients will often express a preference for treatment in primary care to avoid the perceived stigma of treatment in specialist services. OST is recommended initially, with a structured reduction (‘detoxification’) to abstinence the preferred approach. There is no clear clinical rationale for ‘maintenance’ treatment with OST, which is used to reduce the harms associated with risky heroin use. It is possible to taper the dose of the prescribed medication, but short-acting opioids such as codeine are hard to reduce as they are required several times each day and long-acting opioids such as buprenorphine or methadone are more practical.
Clinical experience suggests that patients presenting with dependence on codeine preparations derive most benefit from the use of buprenorphine. Switching the preparation away from the substance that was being misused can be a useful motivating strategy for the patient, and structured dose reduction of buprenorphine has been anecdotally reported to produce fewer withdrawal symptoms. Patients may also be more likely to accept the use of buprenorphine than methadone, which many associate with treatment of heroin dependence. The GP should avoid abruptly stopping a prescription for opioids that is being misused, as this is likely to lead to the patient sourcing opioids from alternate sources such as ‘doctor shopping’ or over-the-counter purchases or by illicit means. Instead, the potential harms should be explained, and a shared management plan aiming towards detoxification should be agreed.
In cases where there is ongoing chronic pain, this process can be more challenging. This situation should prompt a thorough assessment of whether there is an ongoing, underlying cause for the reported pain, with investigations and referral to relevant specialist colleagues where appropriate. If there is chronic pain, optimization of treatment, including non-pharmacological measures, to address the pain is crucial.
Pain Medications in People with Known Substance Misuse
Good management of acute and chronic pain in this population is critical, as poor management can have very serious consequences, including relapse to misuse and addiction, compromised medical care, diversion of opioids to the black market and potentially fatal toxicity due to misjudged tolerance or drug interactions. The stigma associated with addiction is often a barrier to delivery of good medical care. The dilemma for abstinent, former heroin addicts is that there is a risk of relapse to addiction if they are exposed to opioid drugs, but also a risk of relapse if they receive inadequate management of acute pain. When prescribing opioids for people with a past or current addiction it is not always helpful to distinguish between managing chronic pain and managing opioid dependence. The critical issue is structured and individualized care with monitoring of response, and there is often no ‘right answer’ (Bell et al., Reference Bell, Reed, Gross and Witton2013).
Mental Health Issues
Dependence on drugs can be extremely stressful and depressing. The daily routine of waking with withdrawal symptoms, sourcing drugs to relieve the withdrawal and then recovering from the effects of the drugs soon becomes unpleasant. Use of illicit substances can also lead to loss of employment, friends or other social capital that may ordinarily act as a buffer against stress and low mood. Most illicit drugs mimic the symptoms of depression or anxiety, either during intoxication or withdrawal. Another, smaller, group of people uses drugs to alleviate the symptoms of mental ill health, or to cope with traumatic experiences.
Co-morbidity is highly prevalent in both community mental health team (CMHT) and drug treatment populations. In a large UK survey, 44 per cent of CMHT patients reported past-year problem drug use and/or harmful alcohol use, whereas 75 per cent of drug service and 85 per cent of alcohol service patients had a past-year psychiatric disorder (Weaver et al., Reference Weaver, Madden and Charles2003). Most patients with co-morbidity appear ineligible for cross-referral between such services. Large proportions are not identified by services and receive no specialist intervention.
Treatment research into severe and enduring mental illnesses has consistently produced three main findings. Firstly, coexisting severe mental health and substance use disorders are common. Secondly, such dual diagnosis is associated with poor outcomes, including higher rates of relapse, hospitalization, violence, imprisonment and homelessness. Finally, parallel but separate mental health and substance use disorder treatment systems deliver fragmented and ineffective care (Drake et al., Reference Drake, Esscock and Shaner2001). Therefore, in 2002 the Department of Health published a Dual Diagnosis Policy Implementation Guide (Department of Health, 2002), which emphasized the policy of ‘mainstreaming’ such cases. This document made clear that mental health services should ensure that anyone with a severe mental health problem and a substance use disorder were their responsibility and that integrated care was the expected ‘gold standard’ for this group.
However, people with less severe mental health issues and coexisting drug use are often unable to access the care they need. This may be because their mental health problems are insufficiently severe to meet access criteria for mental health services, or because the symptoms are viewed in isolation from substance use. Intoxication may be given as a reason not to offer acute services to people in crisis. An empathic, long-term perspective is required, supporting the individual to reduce and ideally stop their use of drugs in order to properly assess the extent of any underlying mental health disorder. The GP is often in the ideal position to coordinate this care, ensuring good communication between specialist mental health and substance misuse services.
Responding to Family Members Affected by Substance Use Problems
Problematic drug use affects not only those actively using substances but also people close to and concerned about them, including family members and friends. There is evidence of increased psychological symptoms, including severe anxiety and depression, experienced by affected family members who tend to be regular visitors to generic health care services (Ray et al., Reference Ray, Mertens and Weisner2009). One way to reduce the harm caused by addiction problems to others is the provision of direct psychological help to those who are affected, irrespective of whether the relative with the addiction problem is in treatment. An example of such an approach is the development and evaluation of the 5-Step Method to help family members in their own right (Copello et al., Reference Copello, Templeton and Orford2010). The five steps of the method are:
Step 1: active listening to elicit the family member’s experience;
Step 2: the provision of targeted and specific information;
Step 3: an exploration of coping responses;
Step 4: establishing and enhancing social support;
Step 5: discussing any additional needs.
This approach is based on the idea that family member responses can be understood as dilemmas. A clear exploration of the advantages and disadvantages of each coping behaviour can lead to a more informed response by the family member and reduction of the stress experienced. Each family is unique and there is no universally ‘right’ or ‘wrong’ response. This approach has been found to be effective in UK primary care settings (Copello et al., Reference Copello, Templeton and Krishnan2000; Copello et al., Reference Copello, Templeton and Orford2009).
Use of illicit psychoactive drugs is common, and patterns of use are constantly changing. Drug use causes a wide range of physical, psychological and social problems, but its illicit nature means it is heavily stigmatized and requires a high index of suspicion in primary care.
Risk factors for substance use disorders include early life trauma, community disadvantage, poor parenting, peer pressure and individual traits.
Asking whether someone uses illicit drugs is a crucial first step, before going on to determine which drugs, how much and how often, through which route and for how long.
An empathic and non-judgemental approach will yield the best results, and should be combined with the provision of simple harm reduction advice.
Opiate substitution treatment (OST) is an effective way of helping individuals dependent on opiates to stabilize their condition and engage with treatment agencies.
Stimulant drugs, cannabis and novel psychoactive substances are more widely used than opiates, and are often linked to mental health problems.
Psychosocial interventions are the mainstay of treatment for most drug problems, and will require the involvement of a specialist treatment agency.
GPs have an important role to play in identifying and preventing dependence on prescribed or over-the-counter medications. Hypnotics and pain medications are particularly likely to be abused.
Managing pain can be challenging in a patient with a substance use disorder, and the use of ‘universal precautions’ may help prevent a prescribing problem developing.
Treatment of co-occurring mental health and substance use disorders is particularly challenging, and the GP may have a key role in coordinating treatment.