Book contents
- Stahl’s Essential Psychopharmacology
- Additional material
- Stahl’s Essential Psychopharmacology
- Copyright page
- Contents
- Preface to the Fifth Edition
- CME Information
- 1 Chemical Neurotransmission
- 2 Transporters, Receptors, and Enzymes as Targets of Psychopharmacological Drug Action
- 3 Ion Channels as Targets of Psychopharmacological Drug Action
- 4 Psychosis, Schizophrenia, and the Neurotransmitter Networks Dopamine, Serotonin, and Glutamate
- 5 Targeting Dopamine and Serotonin Receptors for Psychosis, Mood, and Beyond: So-Called “Antipsychotics”
- 6 Mood Disorders and the Neurotransmitter Networks Norepinephrine and γ-Aminobutyric Acid (GABA)
- 7 Treatments for Mood Disorders: So-Called “Antidepressants” and “Mood Stabilizers”
- 8 Anxiety, Trauma, and Treatment
- 9 Chronic Pain and Its Treatment
- 10 Disorders of Sleep and Wakefulness and Their Treatment: Neurotransmitter Networks for Histamine and Orexin
- 11 Attention Deficit Hyperactivity Disorder and Its Treatment
- 12 Dementia: Causes, Symptomatic Treatments, and the Neurotransmitter Network Acetylcholine
- 13 Impulsivity, Compulsivity, and Addiction
- Suggested Reading and Selected References
- Index
- References
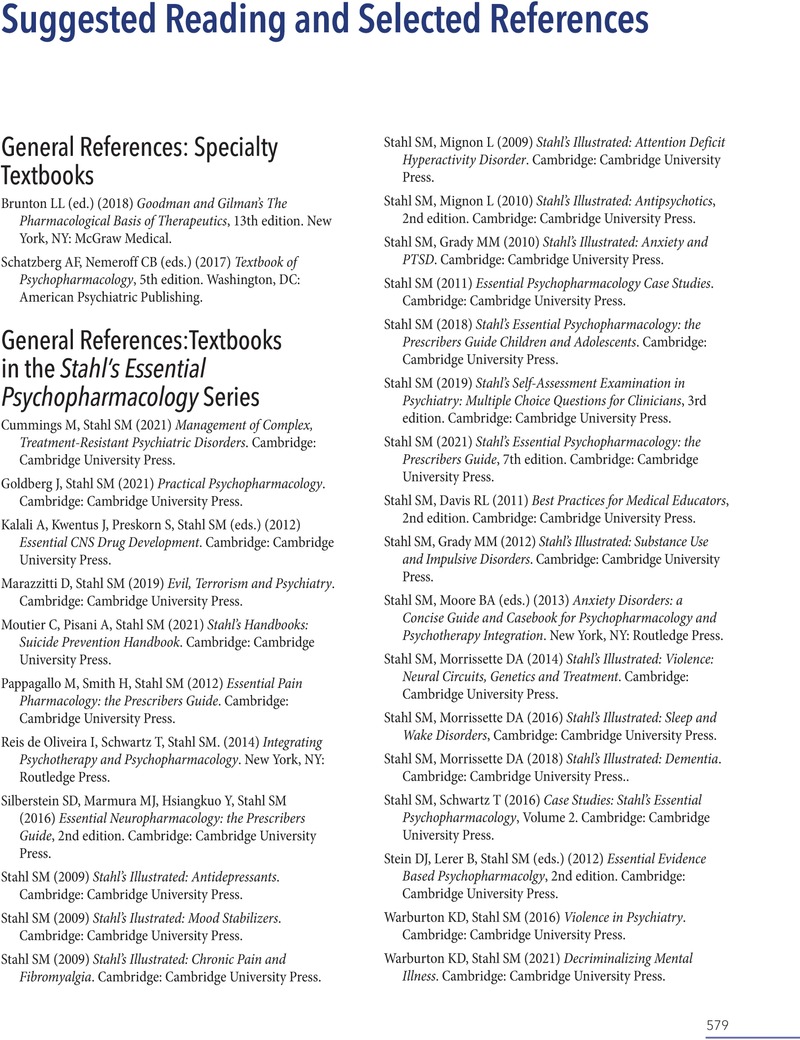
Suggested Reading and Selected References
- Stahl’s Essential Psychopharmacology
- Additional material
- Stahl’s Essential Psychopharmacology
- Copyright page
- Contents
- Preface to the Fifth Edition
- CME Information
- 1 Chemical Neurotransmission
- 2 Transporters, Receptors, and Enzymes as Targets of Psychopharmacological Drug Action
- 3 Ion Channels as Targets of Psychopharmacological Drug Action
- 4 Psychosis, Schizophrenia, and the Neurotransmitter Networks Dopamine, Serotonin, and Glutamate
- 5 Targeting Dopamine and Serotonin Receptors for Psychosis, Mood, and Beyond: So-Called “Antipsychotics”
- 6 Mood Disorders and the Neurotransmitter Networks Norepinephrine and γ-Aminobutyric Acid (GABA)
- 7 Treatments for Mood Disorders: So-Called “Antidepressants” and “Mood Stabilizers”
- 8 Anxiety, Trauma, and Treatment
- 9 Chronic Pain and Its Treatment
- 10 Disorders of Sleep and Wakefulness and Their Treatment: Neurotransmitter Networks for Histamine and Orexin
- 11 Attention Deficit Hyperactivity Disorder and Its Treatment
- 12 Dementia: Causes, Symptomatic Treatments, and the Neurotransmitter Network Acetylcholine
- 13 Impulsivity, Compulsivity, and Addiction
- Suggested Reading and Selected References
- Index
- References
Summary
- Type
- Chapter
- Information
- Stahl's Essential PsychopharmacologyNeuroscientific Basis and Practical Applications, pp. 579 - 614Publisher: Cambridge University PressPrint publication year: 2022